The true cause of 25-60% of pregnancy losses is unknown. Where it is known the causes could vary from medical conditions affecting the baby itself to those affecting the mother.
Tweet
Most pregnancy losses within the first trimester are due to genetic disorders in the baby which are not compatible with life.
Thereafter,
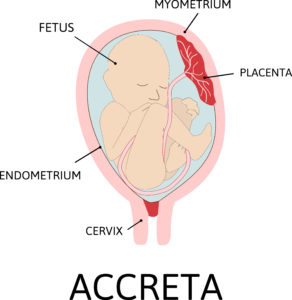
- structural or functional abnormalities with the body of the mother’s womb or placenta or cervix,
- pre-existing medical conditions in the mother such as sickle cell disease, poorly controlled diabetes or hypertension, pre-eclampsia and thyroid disease,
- hormonal imbalances,
- incompatibilities with the mother and baby’s blood group (eg. Rhesus incompatibilities),
- immune diseases such as antiphospholipid syndrome,
- infections and
- trauma are common causes of stillbirth.
Some of these conditions may threaten the ability of the mother’s body to sustain the pregnancy to its completion. They do this directly or cause abnormalities in the unborn baby that may not be compatible with its survival.
What causes miscarriages?
The true cause of 25-60% of pregnancy losses is unknown. Where it is known the causes could vary from medical conditions affecting the baby itself to those affecting the mother.
Why Is Finding Out the Cause Important?
The essence of exploring the causes of pregnancy loss with your health provider (where possible) is to set in motion a plan of action. The aim is to permanently correct any abnormality, manage any chronic condition proactively. Thus, we may be better prepared to forestall a repeat pregnancy loss the next time the mother conceives.
With the guilt that follows miscarriages, some individuals believe that sexual intercourse, strenuous exercise or work can lead to miscarriages. On the contrary, there is no known evidence to support this notion.
What do you Feel When a miscarriage Occurs?
Sometimes a pregnancy loss may be silent ie. the mother may not observe any obvious signs coming to the knowledge of what has occurred during a routine check or after a missed period.
Common symptoms include:
- bleeding of various degrees,
- passage of the fetus or bits of tissue from your vagina,
- abdominal cramps of various degrees, fever,
- lower back pain and loss of previously felt symptoms of pregnancy such as breast fullness, nausea.
Once a total or imminent pregnancy loss is confirmed, your health care provider will need to ensure that your womb is completely empty. This is verified through a series of tests which would include an ultra sound scan as well as give you medication and/or perform a surgical procedure on you.