Ovulation is a stage of the 28-day menstrual cycle. Ovulation specifically refers to the release of the egg (ovum) from the ovary of a female. If the egg is not fertilized during that time, it disintegrates (breaks down), and menstruation (your period) begins approximately two weeks (14 days) later. In this post, you’ll learn all you need to know about pregnancy and ovulation.
Don’t stop reading.
What Is Ovulation?
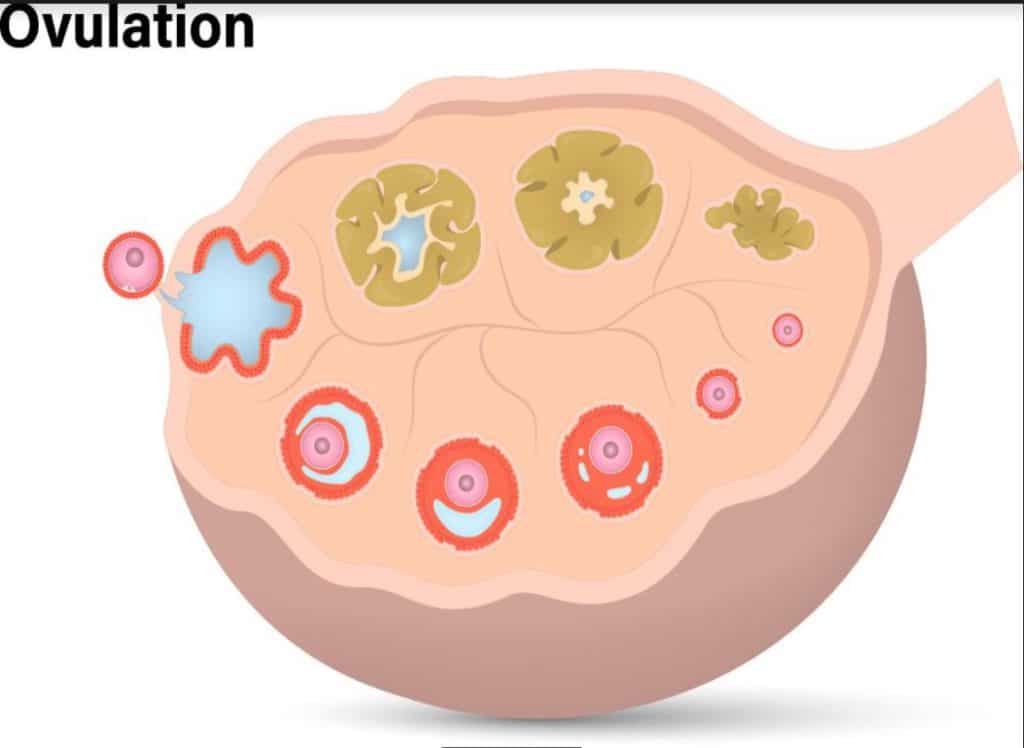
Reproductive hormones cooperate to activate the ovaries during the menstrual cycle, which leads to the development of follicles. Every follicle contains an immature egg. Ovulation is the release of an egg, or ovum, from the ovaries.
In most women, ovulation occurs on the 14th day of the menstrual cycle.
After ovulation, the egg moves through the fallopian tubes and into the uterus. When the sperm and egg come into contact at the proper time, conception may occur.
Signs of Ovulation
There are specific signs and also various methods of detecting ovulation. A proper understanding of these signs and symptoms is helpful while trying to conceive. You can also read this post about 7 interesting signs of ovulation.
These signs include:
1. Fertile quality vaginal discharge
Cervical mucus production is enhanced by an increase in estrogen levels before ovulation. Cervical mucus also undergoes a change in appearance, going from having a stickier, clumpier texture to resembling raw egg whites.
2. Ovulation predictor test strips
Thankfully, there are also tests available that can tell you when ovulation is about to occur, you urinate on the test to acquire a result, they operate similarly to pregnancy tests. This test strip works by detecting luteinizing hormone in your bloodstream.
3. Ovulation monitor
The ovulation monitor is a fancier form of an ovulation test strip. Some digital ovulation monitors utilize urine test strips to evaluate hormone levels, while others determine upcoming ovulation by measuring saliva, cervical secretions, or temperature.

4. Cervical opening
The cervix rises upward, softens to the touch, and opens slightly as ovulation approaches.
5. Basal body temperature
This is the most common method of determining ovulation dates. It depends on software that uses temperature data to track the progress of your menstrual cycle. However, this method is not reliable for women with irregular periods.
6. Typical cycle length
An ovulation calendar can help you determine when you are most fertile. Although it is not 100% accurate, the findings are adequate if you have regular cycles.
Conception and Fertilization
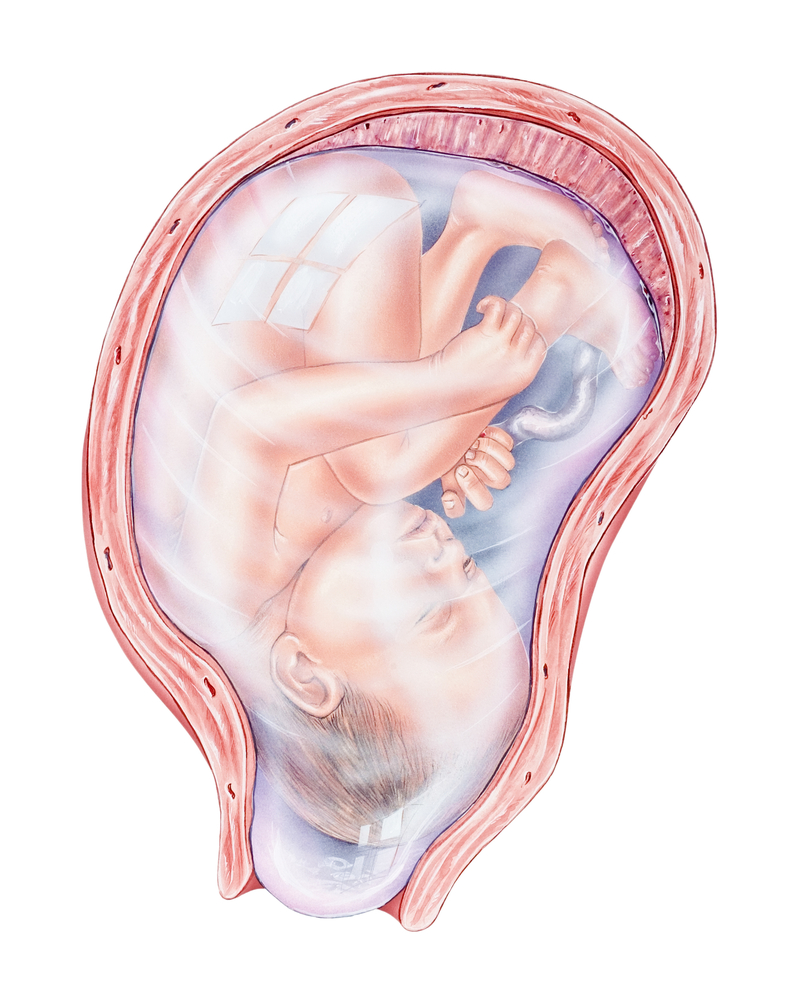
When an egg cell from a woman travels down one of the fallopian tubes from the ovary to the uterus and it combines with a sperm cell from a fertile man as it swims up through the vagina and into the uterus, conception occurs.
You can also read this article on how to calculate your conception date.
An embryo is the product formed when the sperm fertilizes the egg. Interestingly, the baby’s DNA and sex are determined at the time of fertilization. Your child will be a boy if the sperm carries the Y chromosome and a girl if the sperm carries the X chromosome.
The fertilized egg spends about 3 to 4 days in the fallopian tube after fertilization. Within the next 24 hours, this fertilized egg rapidly divides into multiple cells. It continues to divide as it slowly passes through the fallopian tube and enters the uterus.
At this point, your body begins to release various hormones that serve as the basis of a pregnancy test and promote prenatal development.
It is at this stage that a woman experiences a missed period.
Do you stop ovulating immediately after conception?
Yes, ovulation stops after conception.
After ovulation, the absence or failure of fertilization leads to menstruation or periods. On the other hand, if the ovulated egg is fertilized, your body knows that you’re pregnant and stops the process of ovulation. This is because the hormones that cause the various signs of pregnancy also inhibit ovulation.

Furthermore, you won’t have periods while pregnant because the uterine lining remains fixed to ensure proper prenatal development during pregnancy. In the rare instance that you experience periods or heavy bleeding in the early stage of pregnancy, please consult your doctor.
Does Ovulation Happen During Pregnancy?
Although it is possible to get a positive ovulation test result during pregnancy, you cannot ovulate while pregnant.
This only happens in cases of false positive ovulation test results arising from fluctuating hormone levels. Remember, a lot of these home test kits are only about 99% accurate.
Additionally, because pregnancy causes a significant rise in hormone levels, those levels could be a little too high, causing the test to show a positive result for ovulation. Therefore, a positive ovulation test result may simply be the consequence of hormonal changes or, in that case, a flawed test.
Conclusion
Only extensive tests that look for many eggs or ultrasounds that check to see if an egg has been released can provide a 100% guarantee of ovulation. In some circumstances, your body may be just about to become pregnant or, regrettably, just about to have a miscarriage.
Since our biological mechanisms are designed to stop the ovulation cycle once the uterus has a fertilized egg to care for, ovulation stops once an egg is fertilized and the woman is pregnant.