The journey to motherhood is both sweet and demanding. Of course, everyone plans and hopes for things to go the right way. However, this isn’t always the case. At about 39 weeks of pregnancy, most healthy pregnant women will fall into labor on their own.
Most, not all.
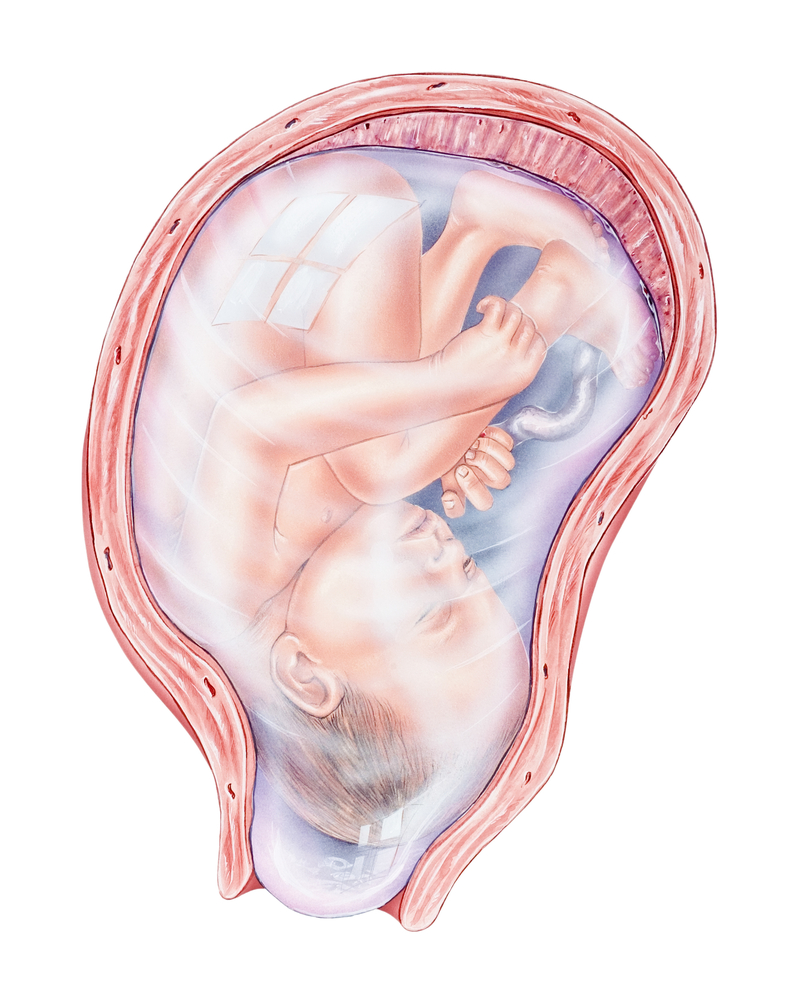
Labor starts with the softening and ripening of the cervix. Once this has happened, the uterus starts contracting, the baby descends as the cervix opens further, the water breaks, and the baby is born. Sometimes, this process doesn’t start spontaneously as expected.
In this instance, healthcare providers could offer induced labor.
What is Induced Labor?
In plain terms, this is the process of artificially stimulating the uterus to begin contractions to achieve a successful vaginal delivery. Generally, doctors perform this procedure before the onset of labor or in situations when the uterus fails to begin contractions by the due date.
In this post, you’d learn all there is to know about induced labor; how it happens, the possible complications, and a final note from us to you.

How long does it take for labor to start after induction?
The time it takes different women to fall into labor after induction varies.
In fact, the onset of labor depends on a number of factors which include:
- The type of induction technique used: The body responds to different techniques in different ways so this will affect the time induced labor will start.
- The position of pregnancy: The position of the pregnancy (first, second, etc) also has a significant effect on the onset of labor. In fact, studies show that induced labor usually takes a longer time if it is the woman’s first pregnancy.
- The gestational age: Pregnancies earlier than 37 weeks take a longer time for labor to begin if induced.
- Ripening of the cervix: The faster the cervix becomes ‘ripe’ i.e. to soften and open, the earlier labor starts.
Most times, induction of labor is an elective procedure.
This means that you would have had enough time to discuss the advantages, disadvantages, and associated risks with your doctor. However, the benefits of inducing labor are usually greater than the risks.
Why Is Labor Induced?
Doctors consider inducing labor for a number of reasons. These include:
1. Post-term pregnancy
Induced labor becomes a valid option if the pregnancy is already more than 39 weeks (at least two weeks more than the due date) and the process of labor has not begun.
2. Ruptured Membranes
Once the water breaks, it is a sign that a baby is ready to come out. However, if labor doesn’t begin soon after, the baby could be in grave danger. As a result, induced labor is a reasonable option in this case.
3. Underlying Maternal Conditions
A history of gestational diabetes or high blood pressure during pregnancy also increases the chances of induced labor. In this instance, labor is induced to monitor fetal health and reduce the risk of complications.
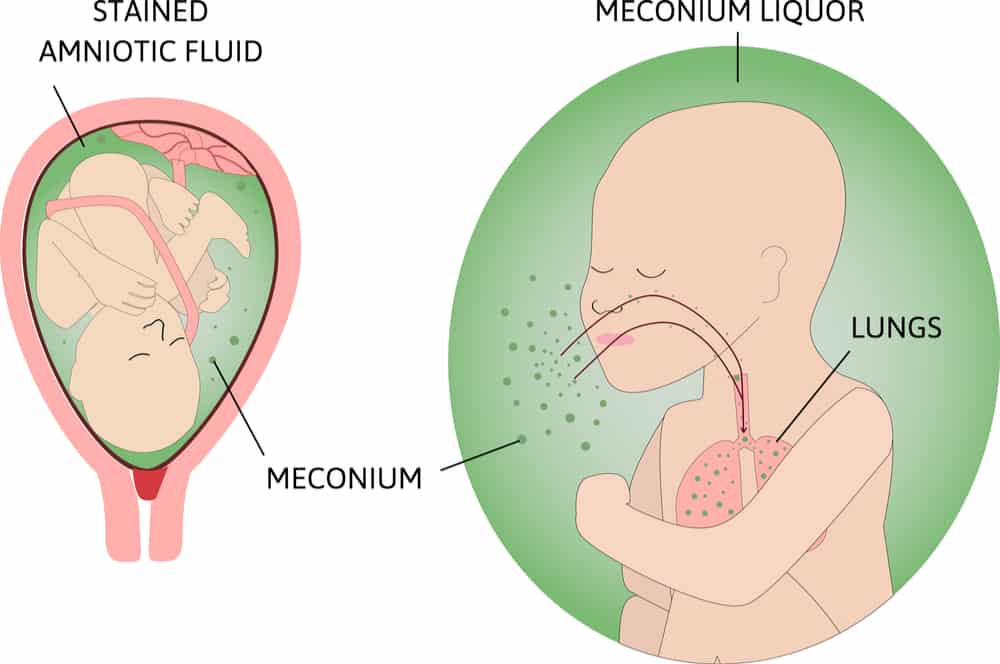
4. Oligohydramnios
This is a reduction in the volume of fluid (amniotic fluid) surrounding a baby. In this case, induced labor hastens the process of labor and reduces the risk of complications.
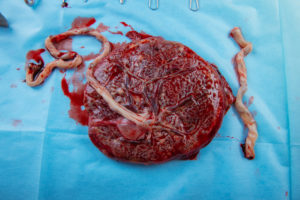
5. Placenta Rupture
This is when the placenta detaches partially or completely from the inner wall of the uterus before delivery. This is not good for babies because there’d be a reduction in nutrients and oxygen supply. As a result, induced labor is a reliable care option.

In addition, induced labor is also a reliable option in cases of:
- Chorioamnionitis
- Intrauterine growth restriction (IUGR)
- Kidney problems
Furthermore, you can also opt for induced labor even if you do not have any of the listed above. This is an option for women with term pregnancies and a history of rapid vaginal deliveries, as it reduces the risk of them going into labor without a healthcare personnel present.
How To Induce Labor
There are different methods of inducing labor. Depending on the need for induced labor, your doctor may:
1. Ripen your cervix
Synthetic prostaglandins can be used to ripen (thin or soften) the cervix. When this is done, your contractions and your baby’s heart rate will be monitored. Also, a catheter (a small tube) with an inflatable balloon on the end is inserted into your cervix. This tube is then filled with saline and it is rested against the inside of your cervix and also helps to ripen your cervix.
2. Rupture your amniotic sac
This technique is also known as amniotomy. It can only be done if the cervix is partially dilated and thinned and your baby’s head is already in the pelvis.
3. Intravenous medication
Your health care provider can give you a synthetic version of oxytocin, known as Pitocin intravenously. (Oxytocin is the hormone that causes the uterus to contract). This can also be used to speed up or augment labor that has already begun.
Your health care provider can use a combination of any of these methods to induce your labor. Usually, induced labor is often successful.
However, if it doesn’t work out as planned, a C-section is the next option.
What are the complications of induced labor?
Some possible complications of inducing labor include:
- Failed Induction: When an indued labor fails, a C-section would be conducted.
- Postpartum Hemorrhage: Induced labor increases the risk of the uterus not contracting properly. This can lead to severe bleeding after delivery.
- Rupture of the uterus: This is possible if you have had a previous uterine surgery.
- Fetal distress: The medications used to induce labor can cause excessive contractions which reduces the baby’s heart rate and oxygen supply, and results in fetal distress.
- Infections: Depending on the technique used to induce labor, such as rupturing the membrane, there may be an increased risk of infection.
A word of caution
Induced labor is not for everyone. It is not an option for you if:
- You have had a previous C-section with a classical incision.
- You have placenta previa (the placenta blocking your cervix).
- Your baby is breech.
- You have an umbilical cord prolapse.
Conclusion
Finally, it is important to remember that induced labors are safe, protected, and often successful. With all the info explained above, you’ve got nothing to worry about.
Remember, we’re always here to help you.
References
Adler, K., Rahkonen, L. & Kruit, H. Maternal childbirth experience in induced and spontaneous labour measured in a visual analog scale and the factors influencing it; a two-year cohort study. BMC Pregnancy Childbirth 20, 415 (2020). https://doi.org/10.1186/s12884-020-03106-4
Lueth, G.D., Kebede, A. & Medhanyie, A.A. Prevalence, outcomes and associated factors of labor induction among women delivered at public hospitals of MEKELLE town-(a hospital based cross sectional study). BMC Pregnancy Childbirth 20, 203 (2020). https://doi.org/10.1186/s12884-020-02862-7