Itching…? Smelly vagina…? Nasty discharge…? Yikes. Unfortunately, women have to deal with a variety of toilet infections occasionally. However, some expectant mothers wonder if they can still get an infection even while pregnant.
We would love to tell you that the answer to that question is no.
Sadly, you can get toilet infections even in pregnancy.

What are the most common infections in pregnancy? What are their symptoms? How do you treat them? How can you protect yourself?
Read on to find out!
Common Toilet Infections In Pregnancy
1) Bacterial Vaginosis (BV)
The vagina has its own bacteria that lives in it naturally.
Bacterial Vaginosis occurs when these bacteria begin to overgrow and multiply more than normal. Sadly, the hormonal changes in pregnancy can influence this overgrowth.

This condition needs to be managed properly to avoid future complications that may affect fertility. In pregnant women, untreated bacterial vaginosis can cause preterm labour, premature birth and low birth weight babies.
Symptoms
- Large amount of thin, grayish-white discharge
- Painful urination
- Irritation/ Itching/ Pain in the vagina or vulva
- Fishy vaginal odor that gets worse after sex
Treatment
If you are pregnant, your doctor would be in the best place to recommend an antibiotic treatment for you.
Furthermore, if you are still early on in your pregnancy, he/she may advice you to wait till second semester before starting treatment.
Prevention
Here are a few things you can do to reduce the risk of you getting an infection;
- Choose comfortable cotton underwear that will allow your vagina to breath and reduce your risk of infection.
- Skip the underwear at night to allow your vagina more room to breath.
- Avoid sitting in wet bathing suits or sweaty panties after swimming or working out. Not only are they uncomfortable, they also make your vagina a perfect bacteria breeding zone.
- Wipe front to back and never back to front after using the toilet. This prevents you spreading bacteria from your anus to your vagina.
- Limit your use of bath oils because they can trap bacteria.
2) Yeast Infection
This is also caused by an overgrowth of a fungus that naturally lives in the vagina.
The hormonal changes during pregnancy creates a suitable environment for the fungus to thrive.
Anything which changes the natural pH (degree of acidity/alkalinity) of the vagina can cause a yeast infection, like taking some antibiotics or having sexual intercourse.
Symptoms
- Painful itching around the vagina or vulva
- Pain or burning in or around the vagina
- Red and swollen vagina
- Thick, whitish-yellow, cottage cheese-like discharge
- An vaginal odor similar to that of bread or beer
- Painful or burning during sex
- Painful urination
Treatment
Yeast infections can be treated with over the counter antifungal medicine. However, pregnant women need to consult with their doctor or midwife before using these medications.
Prevention
- Wear comfortable cotton underwear.
- Sleep without underwear as often as possible
- Drink enough water; at least 8 glasses per day.
- Do not hold your pee. Frequent urination helps eliminate bacteria that can cause infection.
- Reduce the amount of refined sugars you consume.
- Enrich your diet with more yogurt. Yogurt has been proven to enhance digestion and decrease the risk of vaginal infections.
3. Group B Streptococcal Infection (GBS)
Group B streptococcus (GBS) is a bacteria that is commonly found in the body, especially in the vagina and rectum (a part of the intestines).
They are usually harmless and cause no symptoms, except in women with chronic conditions like diabetes or liver disease.
However, caution needs to be taken if you are pregnant as it can be transferred from mother to child. When this happens, GBS could prove harmful and even fatal in a newborn.
Symptoms
This infection may have no symptoms at all, or may be expressed as a Urinary Tract Infection (UTI) in some people.
Common symptoms of a UTI include;
- Painful urination
- Cloudy urine
- Sudden impulse to urinate.
Treatment
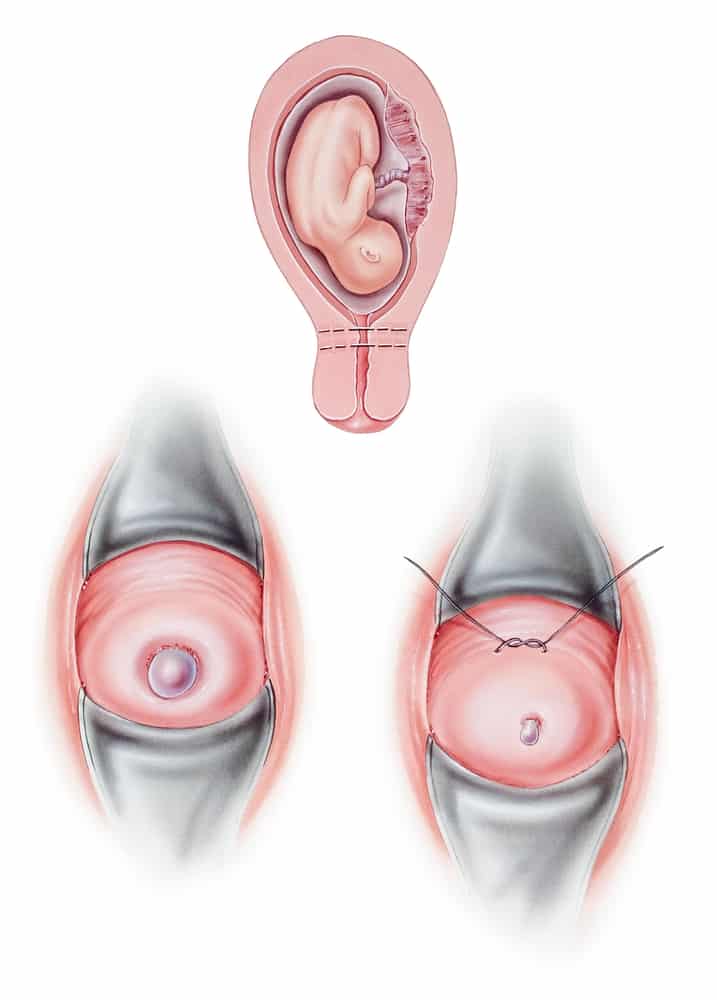
Pregnant women are usually tested for GBS in their last trimester (36 to 37 weeks).
If you test positive, your doctor will administer IV antibiotics during childbirth to prevent you from passing the infection to your baby.
Prevention
Unfortunately, there is no known way of preventing GBS.
However, administration of antibiotics during labour has been shown to reduce the risk of mother-child transmission.
4) Trichomoniasis
This is one of the most common sexually transmitted diseases. Thankfully, it is also one of the most curable.
Although it is transmitted mainly through sex, it can also be gotten from damp or moist towels, clothing or toilet seat that get in contact with the genital area.
Recent research has shown that it can be gotten even from swimming pools!
Symptoms
- Greenish-yellow discharge
- Foamy, foul-smelling discharge
- Itching and burning vagina
- Pain or irritation during sex
Treatment of Toilet Infections
Your doctor will prescribe oral antibiotics to deal with this infection. In addition, it is important to avoid over-the-counter drugs.
Prevention
- Practice safe sex
- Maintain good toilet hygiene
- Avoid sharing towels, under wears or other personal items.
- Frequent testing of you and your partner
How Will These Infections Affect My Baby?
A lot of maternal infections can affect a growing baby in three ways;
- Infections may harm or weaken the mother, making it more difficult for her body to nurture and nourish her child. Also, drugs used in treatment may prove harmful to the baby.
- These infections could not only harm the mother but also directly affect the baby. In severe cases, it can lead to some birth abnormalities.
- Maternal infections can lead to premature labour or a miscarriage.

Therefore, following all the preventive measures above would reduce the risk of you getting an infection or transmitting it to your baby.
In Conclusion,
Your body undergoes a lot of changes during pregnancy, and increased vaginal discharge is one of them.
Although this is normal, sometimes it can be a sign of a toilet infection during pregnancy. If this happens to you, do not be scared.
Most women who get an infection during pregnancy do not have any serious complications. They are easy to treat once diagnosed. To sum it up, if you experience any unusual symptoms while pregnant, speak to your doctor or midwife.
References
- Gonçalves B, Ferreira C, Alves CT, Henriques M, Azeredo J, Silva S. Vulvovaginal candidiasis: epidemiology, microbiology and risk factorsexternal icon. Criti Rev Microbiol 2016;42:905-27.
- “What are the treatments for bacterial vaginosis (BV)?”. National Institute of Child Health and Human Development. 15 July 2013. Archived from the original on 2 April 2015. Retrieved 4 March 2015.
- Zawn Villines 2018, Common infections during pregnancy, Medical News Today, Viewed on Sept 10, 2020, <https://www.medicalnewstoday.com/articles/322210>.
- Shutterstock