The heart is the most vital organ in the body, even in a growing fetus. As a result, it’s very important to monitor a baby’s heart rate and rhythm during pregnancy. In fact, this process involves careful consideration of the various stages of pregnancy and the resulting changes to heart functions.
This way, everyone is sure that your baby is healthy and strong.
In this article, you’d discover all you need to know about fetal bradyarrhythmia, an important heart condition in growing babies. You’d also learn how doctors monitor a baby’s heart rate.
Don’t Stop Reading.

What Is Fetal Bradyarrhythmia?
By the 3rd trimester, the normal fetal heartbeat ranges between 110 to 160 bpm (beats per minute). In most cases, this heart rate remains until labor.
In simple terms, any deviation from the normal heartbeat range of 110-160bpm is an arrhythmia. You should see fetal tachyarrhytmia. Most times, the detection of any form of arrhythmia serves as an indication that the mother or baby is at potential physical risk.
Therefore, fetal arrhythmia is a general term for any form of abnormality in the heartbeat of a fetus.
Examples of arrhythmias include:
- Fetal Bradyarrhythmia: a sustained heart rate that is lower than normal (lower than 110bpm).
- Fetal Tachyarrhythmia: a sustained heart rate that is higher than normal (higher than 160bpm).
- Irregular heart beat
How To Monitor Your Baby’s Heartbeat
As we mentioned earlier, a baby’s heart rate serves as a key indicator of his/her health status before birth. As a result, doctors monitor fetal heart rate during your regular antenatal clinics. This way, any changes can be caught on time to prevent further damage.
The major method of monitoring fetal heart rate is through ultrasonography, where an ultrasound machine is used to observe the baby in the womb.

Another means is through the use of an internal device that is directly connected to the baby’s scalp. This method helps to measure the fetal heart rate more accurately but can be uncomfortable for the mother.
How Does My Baby’s Heart Beat?
A baby’s heart, like an adult’s, beats by a series of electrical activities which spread throughout the walls of the heart. These electrical signals are generated from the sino-atrial(SA) node, which functions as the natural pacemaker of the heart.
The SA node is called the pacemaker because it sets the rate and rhythm of the heartbeat.
Generated impulses are conducted from the SA node to the chambers of the heart (atria and ventricles). Contraction of the atria and ventricles in response to transmitted electrical impulses is what results in a heartbeat.
As we mentioned earlier, bradyarrhythmia occurs when the heartbeat process occurs a lot slower than it should.
What Causes Fetal Bradyarrythmia?
Generally, fetal arrhythmias are very uncommon, affecting only about 1-2% of all pregnancies. However, when they occur, they are often a result of problems associated with the heart’s electrical conducting system.
The main cause of low heart rate in a fetus is a problem with the sino-atrial node of the heart. The sino-atrial node (SAN) is the natural pacemaker of the heart where electrical impulses that make the heartbeat are generated. Another cause could be a problem with the transmission of these impulses from the upper chamber of the heart to the lower chamber.
Other Associated Conditions
Most times, fetal bradyarrhythmia doesn’t walk alone. It may be linked to any of the following maternal or child health conditions:
- Congenital heart defects
- Maternal lupus
- Chromosomal abnormalities e.g Trisomy 18 (Edwards’ syndrome)
- Maternal hypotension
- Sjogren’s syndrome
Types of Fetal Bradyarrhythmia
Depending on the severity, fetal bradyarrhythmia may be classified into the following groups:
1. Sinus Bradyarrhythmia
This is a form of slow heartbeat which is often asymptomatic. Furthermore, this form of bradyarrhythmia is transient, as it resolves on its own.
In sinus bradyarrhythmia, the heartbeat is generated in the sino-atrial node but is slower than normal (less than 110bpm). As we mentioned earlier, this is due to the improper functioning of the heart’s pacemaker, the sino-atrial node.
Sometimes, the condition is temporary and may result from excess pressure on the uterus.

In other instances, sinus bradyarrhythmia can be an indication of fetal distress such as lack of oxygen. In such cases, doctors perform an emergency cesarean section to save the baby. However, mild sinus bradyarrhythmia often requires no form of treatment.
2. Atrioventricular block
In other instances, this is termed a 1st-degree heart block.
It occurs due to a delay in the transmission of electrical impulses between the chambers (atria and ventricles) of the heart.
3. Partial Atrio-ventricular block
2nd-degree heart block is another name for a partial atrio-ventricular block.
In this instance, there’s partial or complete interruption of the transmission of electrical impulses from the atria to the ventricles. This makes the heart beat slowly or skip some beats.
4. Complete heart block
In other instances, this is termed a 3rd-degree heart block.
When this happens, electrical impulses from the atria do not reach the ventricles at all. In order to compensate for the lack of signal, the ventricles act as a substitute pacemaker and generate impulses on their own.
However, the signals generated by the ventricles are weaker, irregular, and not reliable. As a result, the heartbeat becomes slower, leading to bradyarrhythmia.
Diagnosis of Fetal Bradyarrhythmia
Thankfully, fetal bradyarrhythmia is detectable during routine maternal ante-natal clinics when the doctor listens to the fetal heart rate with an ultrasound machine.
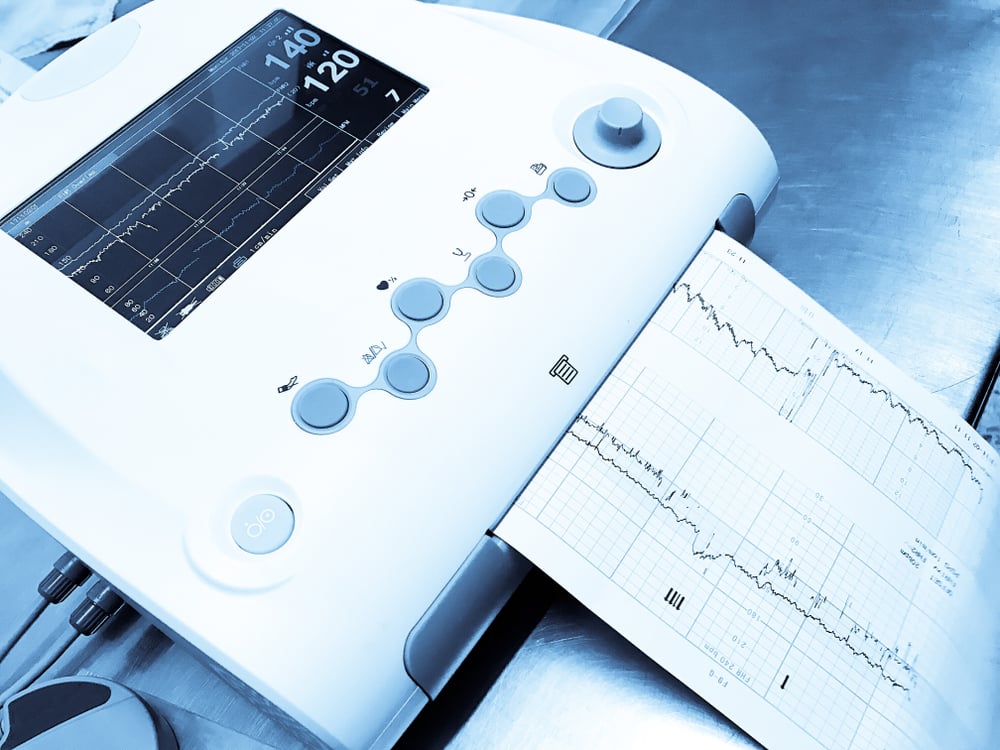
In the case of an abnormal heart rhythm, a comprehensive examination to confirm the diagnosis is necessary. This comprehensive exam is to evaluate fetal movement, tone, and amniotic fluid volume.
How Risky Is Fetal Bradyarrhythmia?
Although mild cases of bradyarrhythmia are not harmful to the fetus, severe cases can be life-threatening.
In severe cases, the fetus suffers a higher risk of developing heart failure and non-immune “Hydrops fetalis”. Hydrops fetalis is a serious condition characterized by the abnormal build-up of fluid in two or more body areas of a fetus. If this condition develops, labor is induced and the baby is delivered immediately.
The Treatment Of Fetal Bradyarrhythmia
As we mentioned earlier, mild cases of fetal bradyarrhythmia require no form of treatment or therapy. However, the fetal heart rate should be closely and regularly monitored until the condition has fully resolved.
For more serious cases of fetal bradyarrhythmia, the treatment plan includes:
- Medications given to mother to increase heart rate e.g beta-sympathomimetic drugs
- Use of steroids to hasten development of the baby’s lungs in case there is a need for preterm delivery.
- Emergency delivery in case of fetal distress.
Delivery
Emergency delivery of a fetus with bradyarrhythmia is a delicate process. In fact, it should only occur in a tertiary hospital with medical workers skilled in postnatal cardiac care. This is because the delivery and postnatal care of patients with this condition involve a team of special cardiologists, pediatricians, and nurse practitioners.
In most cases, especially when the baby is at risk, a cesarean section is the safest option.
Postnatal Care
As expected, the treatment plan after birth is based on each child’s arrhythmia and the presence of underlying conditions. In mild cases, the heart rate may resolve on its own without treatment. In other cases, patients may require some sort of medication for proper treatment.
Furthermore, mothers with underlying connective tissue diseases, like rheumatoid arthritis or lupus, should follow up on their routine treatment plan after delivering a baby with fetal bradyarrhythmia.
Conclusion
In conclusion, it’s really helpful to remember that most cases of fetal bradyarrhythmia are not life-threatening. In fact, with proper management and care, both the mother and child are going to be just fine.