Your maternity leave is about to end. Maybe you need to go on a trip without your baby. You’ve been breastfeeding directly all this while. Time to switch to bottle feeding and your baby outrightly rejects the bottle at your first attempt.
The clock is ticking and your baby still doesn’t want a bottle.
Your resumption date is fixed or your flight ticket has been booked. In fact work has started coming in , in anticipation of your arrival at the office.
Nope.
This isn’t the opening narration of a horror movie. Neither is it the work of your enemies. It’s legit the reality of some working mums in Nigeria.
How do I get back to work and continue feeding a baby that’s rejecting the bottle????
First things first. Please read our guides to selecting bottle teats and how to know if your baby is getting enough milk.
Done?
Now let’s continue the discussion below.
As a mum who want to breastfeed exclusively it’s advisable to delay bottle feeding till your baby is 4 weeks old and you have established breastfeeding properly (gotten your latch right etc etc).
That said…..
Sometimes, you may need to delegate feeding to rest or return to work outside the home when maternity leave ends.
For this, consider selecting a bottle with teats that look similar to your nipples when you are doing your baby shopping.
Despite your best effort, some babies just don’t like bottles .
In this case, consider feeding with any of these alternatives to bottle feeding:
- Cup and spoon
- Small Syringe (without the needle please, ejo, mbok, biko )
- Feeding cup

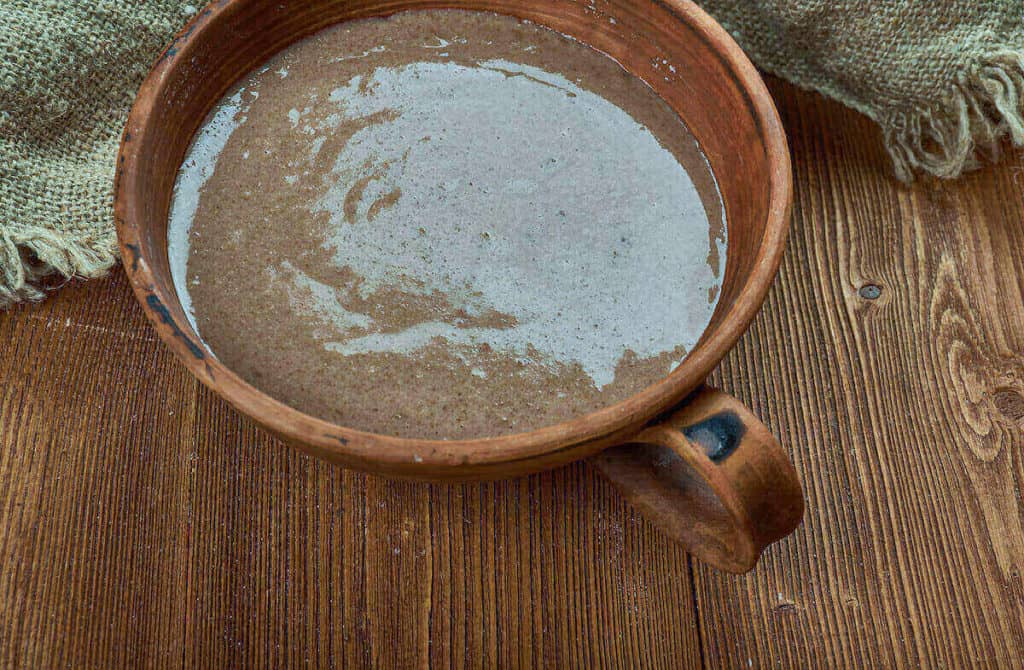
Feeding Cup 
Cup or bowl and spoon
These methods require that your baby is held a bit upright and fed patiently to avoid choking.
Please delegate this task to someone who is diligent and careful .
If you liked the tips in this article, you’ll love our guide to exclusive breastfeeding with a 9-5 job.