Breast milk is an essential source of nutrition for newborns and infants, and it is common for mothers to notice specific changes in the makeup of their milk. The smell of pumped, high-lipase breast milk is one of these differences. This article will examine high lipase breastmilk in detail, along with its causes, effects, and management options.
What is lipase?
Lipase is a vital enzyme that aids in the breakdown of breast milk so that your baby can digest and absorb its vital nutrients.

Breast milk contains lipase naturally, and it is thought that too much of this enzyme can alter the taste of breast milk.
What is High Lipase Breastmilk?
Lipase helps the baby digest the milk properly. However, when the levels of lipase enzymes are too high, the milk can develop an unpleasant, soapy taste and smell. High lipase breast milk is breast milk that has high levels of lipase enzymes. High lipase levels are believed to cause the fats in your milk to break down more quickly when stored at cool temperatures, affecting the flavor and odor.
How Common is High Lipase Breastmilk?
High lipase breast milk affects a small percentage of nursing mothers. The exact prevalence of this condition is unknown, but some studies suggest that up to 15% of women may experience high lipase breast milk.
Why do I have high-lipase milk?
Let us clarify that breast milk with a high lipase activity level does not necessarily mean something is wrong with you. It does not mean you’re a failure or something is physically wrong with you.
Breast milk contains an enzyme called lipase that helps with fat digestion and absorption. The cause of high lipase in breast milk is not entirely clear. Some research suggests that it may be due to genetics, while others believe an excess of the hormone prolactin may cause it. Breast milk could develop a high lipase content for no apparent reason. Simply put, some mothers’ breast milk contains too much lipase while others do not.
How to Test if my Breastmilk Has High Lipase Levels?
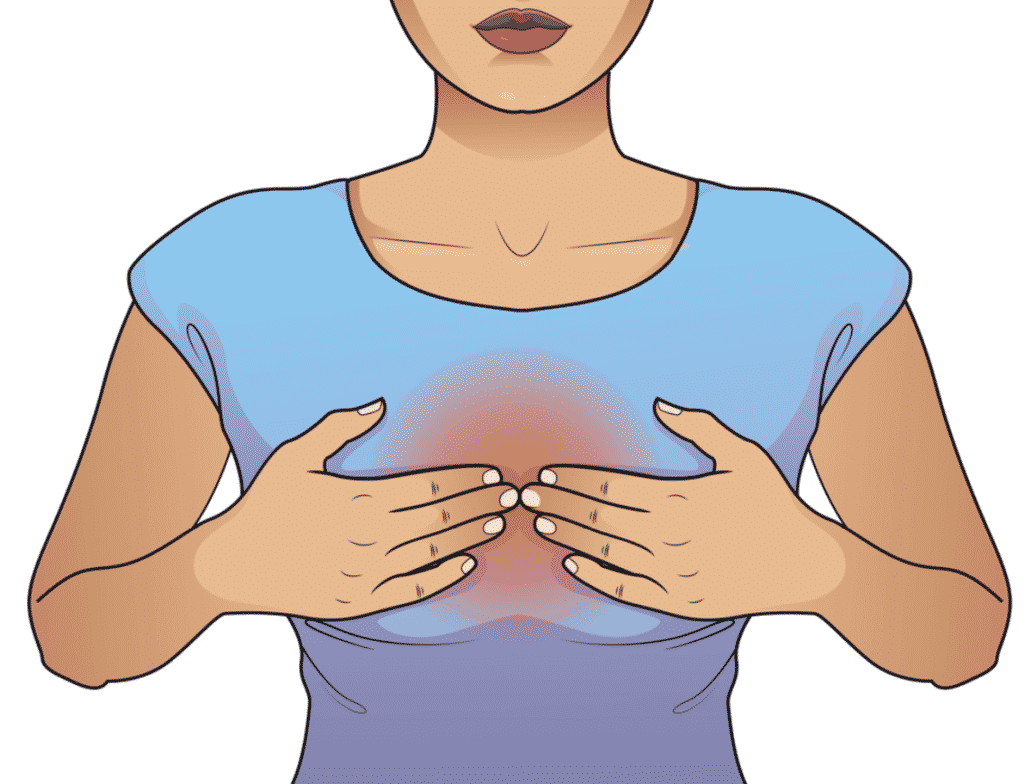
Yes, you can and should taste your breast milk. To test for high lipase breastmilk, express a small amount of milk and smell it. You can also try tasting the milk to determine if it has an unusual flavor. If the milk has a sour or soapy smell, it likely has high levels of lipase enzymes.
What do I do if I have high lipase breast milk?
It is important to understand that your baby will not be harmed if you are a lactating mother with high lipase levels in your breast milk. High lipase levels, however, can give your breast milk a sour or soapy taste, which might make it challenging for your baby to eat. Following are some actions you can take:
- Consult your doctor: If you are worried about your lipase levels, it is essential to talk to your doctor, who can help you identify the underlying cause.
- Try various feeding methods; Some babies might prefer to feed from the breast rather than a bottle because it can reduce exposure to milk with a high lipase level.
- If scalding your breast milk is not an option, you might think about storing it in breast milk storage bags and freezing it as soon as you express it. This can lessen the impact that high lipase has on milk flavor.
Remember that while high lipase levels in breast milk can affect the flavor of your milk, they are not harmful to your baby. You can lessen the adverse effects of high lipase on your breastfeeding experience by attempting to scald your breast milk and experimenting with various feeding methods.
You can try warming it to room temperature or mixing it with fresh breast milk. Some mothers also find success in mixing high-lipase breastmilk with formula or with foods like cereal or oatmeal or using it as the base for smoothies; these options are only suitable for children that are weaned.
How to Store High Lipase Breastmilk?
To preserve high-lipase breastmilk, You can freeze it for up to six months, but using it as soon as possible is best.
Is the Health of my Baby Affected by High Lipase Milk?
Clinical research does not support high-lipase breast milk’s short- or long-term effects on an infant’s health. Additionally, there are no known adverse effects. Lipolysis only causes the flavor and taste of milk that has been stored to change.
It might imply that your baby will benefit from these changes. Indeed, a study demonstrated that lipase in breast milk could replace pancreatic lipase functions during infancy, promoting healthy growth, especially in preterm infants.
In conclusion,
High lipase breast milk is a common condition that affects some nursing mothers. While it can cause stress and anxiety for the mother, it is essential to remember that the milk is still nutritious and safe for the baby to consume. Mothers can ensure that their babies receive the best possible nutrition by understanding what high lipase breastmilk is, how to test for it, and how to store and use it properly.
If you are struggling with high lipase breast milk, do not hesitate to contact a lactation consultant or your healthcare provider for support and guidance.