Sharon has dealt with the pain all her life. In fact, she still had a sickle cell crisis a few weeks before the pregnancy test results came in positive.
Women like Sharon often wonder how to deal with pregnancy due to the risks associated with their genotype. Thankfully, due to the major advancements in medicine, it has become possible for women with Sickle Cell Disease to triumph through pregnancy and delivery process.
What Is Sickle Cell Disease?
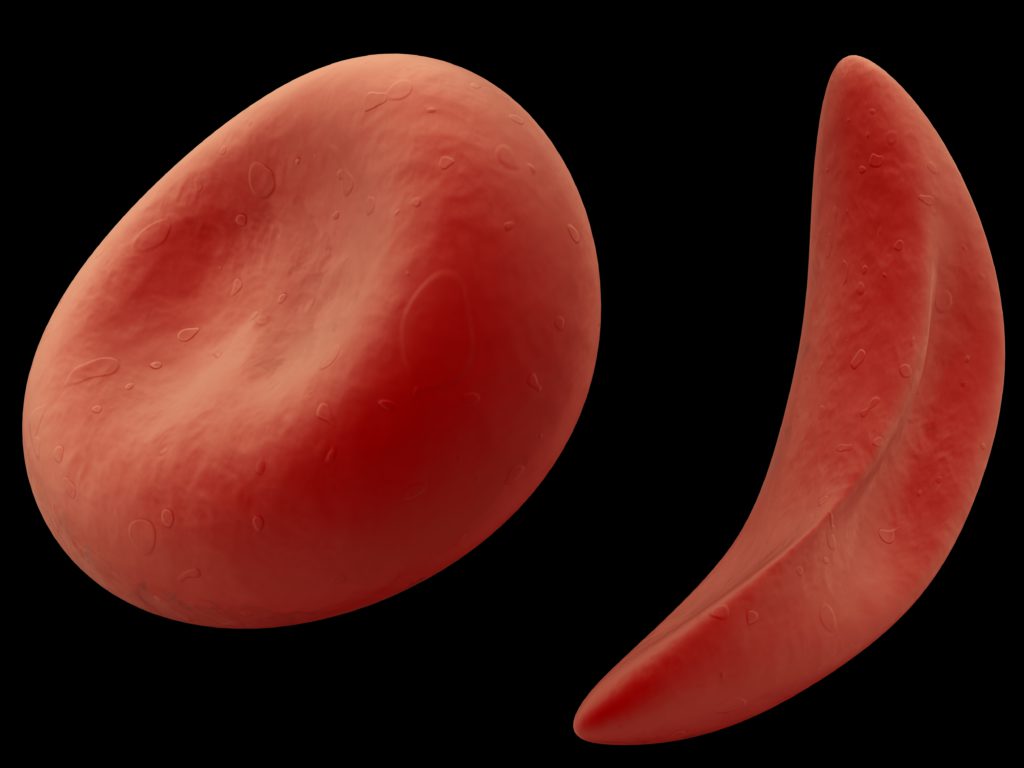
Sickle cell disease (SCD) is an inherited genetic condition in which the body produces abnormally shaped red blood cells under stressful conditions. These abnormal red blood cells can be C-shaped or sickle-shaped. They have a high tendency to stick to each other.
They also aren’t as flexible as the normal shaped cells making it difficult to navigate tight corners in tiny or branching blood vessels and so on.
These cause blockages cutting off blood supply to areas where the vesses were orignally headed.
This is the cause of the excruciating pain and damage to tissues and organs that have their oxygen supply cut off. Such events are the cause of strokes bone infections and and so on.
Effects of SCD on Pregnancy
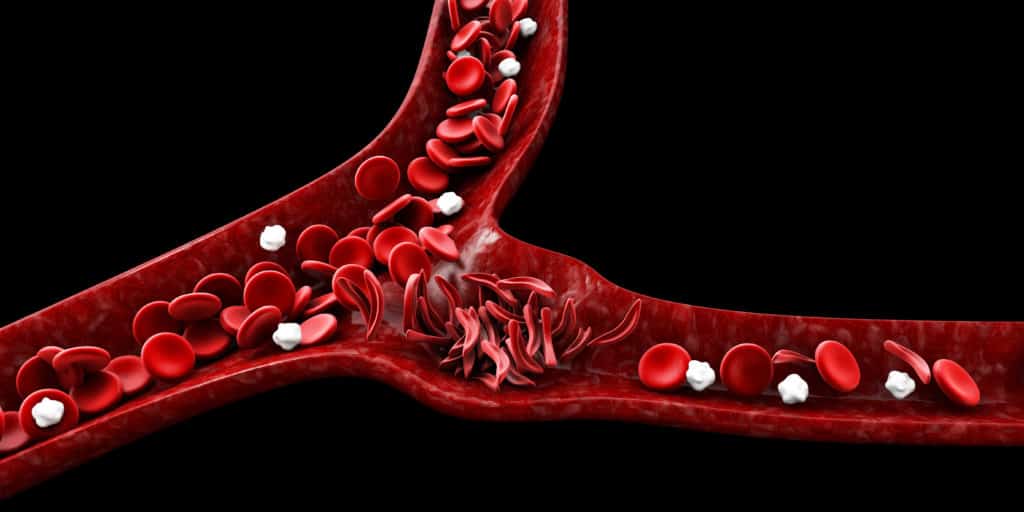
- Sickle Cell Crisis. This is also known as painful episodes. It occurs when a sickle-shaped or C-shaped red blood cell block blood vessels that supply blood to the bones. This crisis can last several hours to several days. And it varies in severity depending on the person and the crisis. The crisis can occur in pregnancy due to the increased physical stress the mother is passing through.
- Anaemia. Anaemia is a condition in which the body does not have enough healthy red blood cells. This results in a reduced supply of oxygen to the various organs of the body. Pregnant women with SCD are at a higher risk of experiencing anaemia during pregnancy that at other times.
- High Blood Pressure. Women with SCD are at risk of developing high blood pressure and preeclampsia (a pregnancy complication characterised by high blood pressure and organ injury ) during pregnancy.
- Women with SCD are at risk of some pregnancy complications. These complications include miscarriages, low birth weight, and pre-term delivery.
- Women with SCD are more likely to deliver through a caesarean section rather than a vaginal birth due to the increased complications associated.
I have Sickle Cell Disease…..What should I do?
Living with sickle cell disease means that you will need special care and attention during your months of pregnancy. You will also need to maintain a good diet and stay hydrated in order to stay healthy. When you are ready, your pregnancy needs to be planned for. You should be managed at a specialised center by a team of health personnel such as – blood specialists (haematologists), obstetricians etc.
A few tips…
- Some of the medication you were on before pregnancy such as hydroxy urea or ACE inhibitors may not be compatible with pregnancy. Please inform your doctor 3 months before you plan on getting pregnant so adjustments can be made.
- Your antenatal check-ups may be more frequent than other pregnant women without SCD. This is because of the nature of your health and the need to stay ahead of any complication that is likely to occur.
- Apart from your routine pregnancy medication, you may be prescribed with some medication ( tablets and/or injections) to be taken throughout pregnancy. These are to prevent crises, and conditions such as pre- eclampsia.
- Be careful of the medication you use. Don’t use any drug without informing your doctor. This is because not all drugs are safe during pregnancy. Therefore, ensure to take only prescribed medication.
- There may need to receive one or more blood transfusion during pregnancy. This can serve as a prophylactic measure (prevention) to prevent complications.
- Because of the nature of the disease, people with SCD usually have excess iron stored in their blood – even when they’re anaemic. Pregnant women in this condition may need to take prenatal vitamins that do not contain iron.

Conclusion
You can have a healthy pregnancy and a safe delivery even with SCD.
Follow your doctor’s guide and instructions. Be sure to be in close and frequent communication with your doctor while pregnant. This will help in close monitoring of your health and early detection of any complication that may want to arise.
REFERENCES
- Royal College of Obstetrics and Gynaecologists (2017). Management of Sickle Cell Disease in Pregnancy. Accessed on 28th August, 2020 from https://www.google.com/url sa=t&source=web&rct=j&url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1324/&ved=2ahUKEwiwyj–rXrAhXXiVwKHXLjCwoQFjASegQIBAB&usg=AOvVaw1Ud_P6KdVyexkOy44esNL7