VAGINAL DISCHARGE DURING PREGNANCY: WHEN SHOULD YOU WORRY?
The journey from pregnancy to childbirth is quite exciting. However, it can also be confusing for first-time mothers.
Your body is going through a lot of changes during this period and it may be difficult to tell what’s normal and what isn’t normal.
One of such changes is your vaginal discharge, which can change during pregnancy.
To a large extent, these changes are normal. However, they may also serve as an indicator of a problem. This would definitely raise the question: When should I begin to worry?
To answer this, you need to know when not to worry. This begins with knowing what is normal.

WHAT IS NORMAL?
It is normal to have discharge whether you are pregnant or not.
However, pregnancy hormones affect your discharge in many ways. You may notice this change shortly after conception, even before you realize you are pregnant.
A healthy vaginal discharge ranges from;
- Clear to milky white.
- Thin to thick or mucus-like.
- Mild-smelling or odourless.
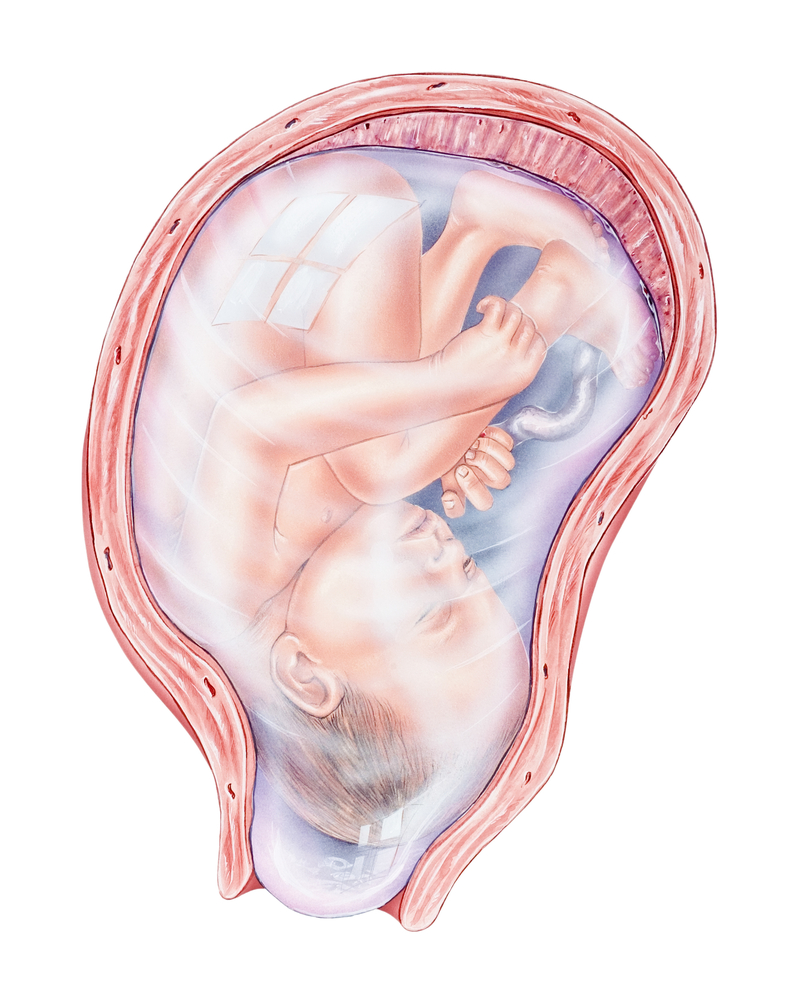
Your discharge would become more noticeable as your pregnancy advances. The closer you get to your delivery date, the heavier your discharge would get. You may have to wear a panty liner. It is best to use an unscented one.
Also, avoid tampons.
Your discharge may contain streaks of blood in the last weeks of pregnancy. Do not panic if this happens. It is just an early sign of labor and is no cause for alarm.
WHAT IS ABNORMAL?
Abnormal vaginal discharge can be a sign of a bacterial or yeast infection. It may also be a symptom of a sexually transmitted disease (STD). If you are pregnant, it can serve as an indicator that something is wrong with the pregnancy.
You should be concerned if your discharge;
- is yellow, green, or gray in color
- has a strong and foul odour
- comes with redness, itching or swelling
- causes pain or soreness during urination or sex
- changes drastically in quantity, colour and texture.

WHAT CAN YOU DO?
There is little you can do about normal vaginal discharge. Some women find it helpful to wear panty liners. Others may find it irritating. Whichever side you are on though, never resort to using tampons. They are highly discouraged during pregnancy.
Nevertheless, there are some little things you can do to keep your private area healthy. Some of them are;
- Wipe properly; from front to back after using the loo
- Change your clothes immediately after working out or swimming.
- Reduce wearing tight pants, leggings or underwear, especially those made with synthetic materials. Wear more loose fitting clothing and cotton underwear.
- Always keep your genital area dry.
- Avoid scented pads or panty liners, bubble baths, deodorant soaps, or any other thing that may irritate your already sensitive skin.
- Please, as tempting as it may be, do not douche. It disrupts the normal vaginal environment and increases your risk of getting an infection.
- If you do develop an infection, consult your health care provider. A suitable vaginal cream or pessary may be recommended for you.

Your vaginal health is very important during pregnancy. Do not take it lightly. There is no need to be ashamed to voice out any concerns you may have about your discharge.
Speak to your health care provider about any changes that may worry you. They are always there to help you and your baby.
REFERENCES
- Juliann Schaeffer 2019, Vaginal Discharge During Pregnancy: What’s Normal?, Healthline, Viewed on July 27, 2020, <https://www.healthline.com/health/pregnancy/vaginal-discharge-during-pregnancy#1>.
- Karisa Ding 2017, Vaginal Discharge During Pregnancy, Babycenter, Viewed on July 27, 2020, <https://www.babycenter.com/0_vaginal-discharge-during-pregnancy_270.bc>.
- Tamekia Reece 2020, Vaginal Discharge During Pregnancy, Healthline, Viewed on July 27, 2020, <https://www.parents.com/pregnancy/my-body/pregnancy-health/discharge-during-pregnancy-whats-safe-whats-not/>.
- Shutterstock