Do you know that high blood pressure is one of the leading causes of complications and death during pregnancy?
Wait!
When last did you check your blood pressure?

As a mum-to-be, it is necessary to monitor your blood pressure regularly. As a result of the new life growing in your tummy, your body works extra hard to meet the growing demands. Sometimes, this may lead to an over-stretching of your systems.
In this article, you’d find helpful tips on hypertension; the types, treatment, and possible complications during pregnancy.
What is High Blood Pressure?
High blood pressure also is also known as hypertension.
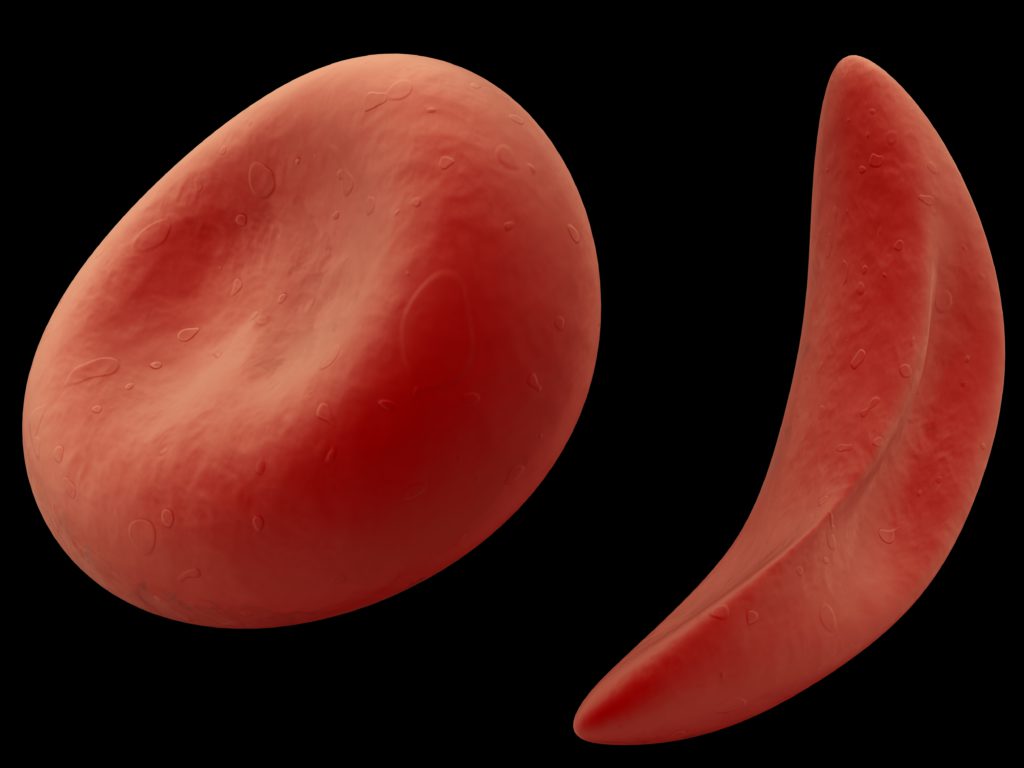
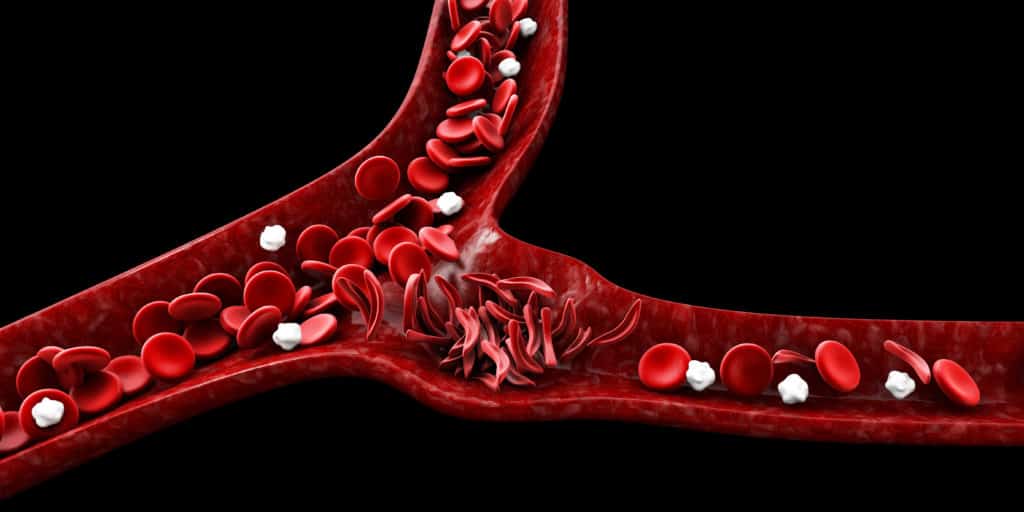
Hypertension is a sustained rise in blood pressure that occurs as a result of several factors. Severe or uncontrolled hypertension during pregnancy can cause complications for you and your baby.
It is also important to note that high blood pressure can occur before, during, or after pregnancy.
Types of High Blood Pressure During Pregnancy
1. Gestational Hypertension
This type of high blood pressure develops after 20 weeks of pregnancy. Gestational hypertension usually goes away after childbirth but it can increase the risk of developing hypertension in the future. Thankfully, in this case, there’s no sign of possible organ damage. However, women with gestational hypertension may develop preeclampsia.
2. Chronic Hypertension
In this instance, the rise in blood pressure was present before pregnancy or before the 20th week of pregnancy. That is to say, the pregnant woman in question is a known hypertensive patient.
3. Preeclampsia
Whenever a sustained rise in blood pressure is observed after the 20th week of pregnancy; it is termed preeclampsia. It is usually associated with signs of damage to other organ systems.
Complications of High Blood Pressure in Pregnancy
1. Restriction Of Your Baby’s Growth
Hypertension can decrease the flow of nutrients to the baby through the placenta resulting in slowed or decreased fetal growth.

2. Preeclampsia
The chances are higher for women with high blood pressure to develop preeclampsia compared to women who have normal blood pressure.
3. Preterm Delivery
High blood pressure may stimulate early labor, leading to preterm delivery. Furthermore, the risk of preterm labor is increased if the baby doesn’t get enough nutrients and oxygen.
4. Caesarean Delivery
A woman with high blood pressure may have to undergo a Caesarean birth. This helps to relieve the stress of vaginal birth and prevent possible birth-related complications.

5. Organ Damage
When hypertension is not properly managed, it can result in potentially life-threatening injury to the brain, lungs, heart, liver, and some other major organs.
6. Postpartum Hypertension
A woman is at risk of postpartum hypertension, i.e. hypertension that starts after delivery if she had high blood pressure during pregnancy.
Managing Hypertension During Pregnancy
Some of the drugs used to manage hypertension are safe and can be used during pregnancy. On the other hand, some medications pose a serious threat to the mother and a growing baby during pregnancy.

Furthermore, it is necessary that you consult your doctor to prescribe the best drugs to manage hypertension in this period.
In Conclusion,
It is important that you follow your doctor’s prescription during pregnancy. Don’t stop using a drug on your own accord and don’t self-medicate.
Finally, it is really important to stay healthy for you and your baby. Stay strong and stay healthy always to avoid a case of threatened abortion.
REFERENCES
- Stephanie Braunthal and Andrei Brateanu (2019). “Hypertension in pregnancy: Pathophysiology and treatment.” Sage Open Medicine. Accessed on 24th September 2020 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6458675/#__ffn_sectitle
- Reem Mustafa, Sana Ahmed, Anu Gupta and Rocco C. Venuto (2012). “A Comprehensive Review of Hypertension in Pregnancy.” Journal of Pregnancy. Accessed on 24th September, 2020 from https://doi.org/10.1155/2012/105918
- Tooher J, Chiu CL, Yeung K, Lupton SJ, Thornton C, Makris A, O’Loughlin A, Hennessy A, Lind JM (2013). “High blood pressure during pregnancy is associated with future cardiovascular disease: an observational cohort study.” BMJ Open. Accessed on 24th September, 2020 from https://bmjopen.bmj.com/content/3/7/e002964