There’s so much to discover while expecting your little one; from your baby bump to the placenta and even your baby’s milestones. In fact, as you progress on this journey, you’d realize that every pregnancy is unique.
In this article, you’d discover everything you need to know about an important medical condition, called placenta previa, which affects the placenta during pregnancy.
Table of contents
What is Placenta Previa?
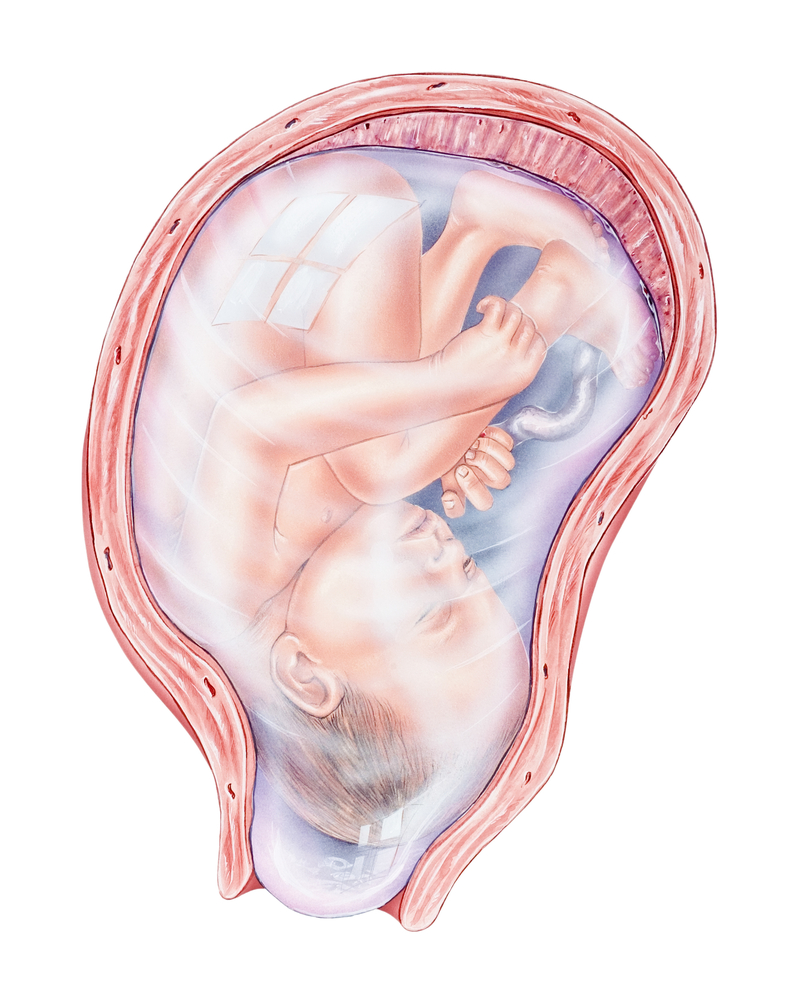
Placenta previa is a medical condition that occurs in a pregnant woman when the placenta blocks the cervix (opening into the birth canal), thereby obstructing the path that the baby should come out from.
In normal conditions, the placenta is attached to the top of the uterus. This way, it can serve as a safe passageway of substances to and from the baby. However, in placenta previa the placenta covers the cervix, causing serious bleeding from the vagina.

Placenta Previa Symptoms
The most common symptom of placenta previa is bleeding.
In fact, 5 in 10 women with placenta previa experience light to heavy bleeding at some point. Medical experts agree that any bleeding during pregnancy may be associated with problems with the placenta. Whenever this bleeding occurs in the second trimester of pregnancy, it may be a symptom of placenta previa.

In most cases, the bleeding is painless, and it can be light, or heavy.
Some women also complain of tightness or cramps due to increased contractions or pressure on their backs while managing placenta previa.
What Are The Types of Placenta Previa?
Depending on the location of the placenta, placenta previa is grouped into:
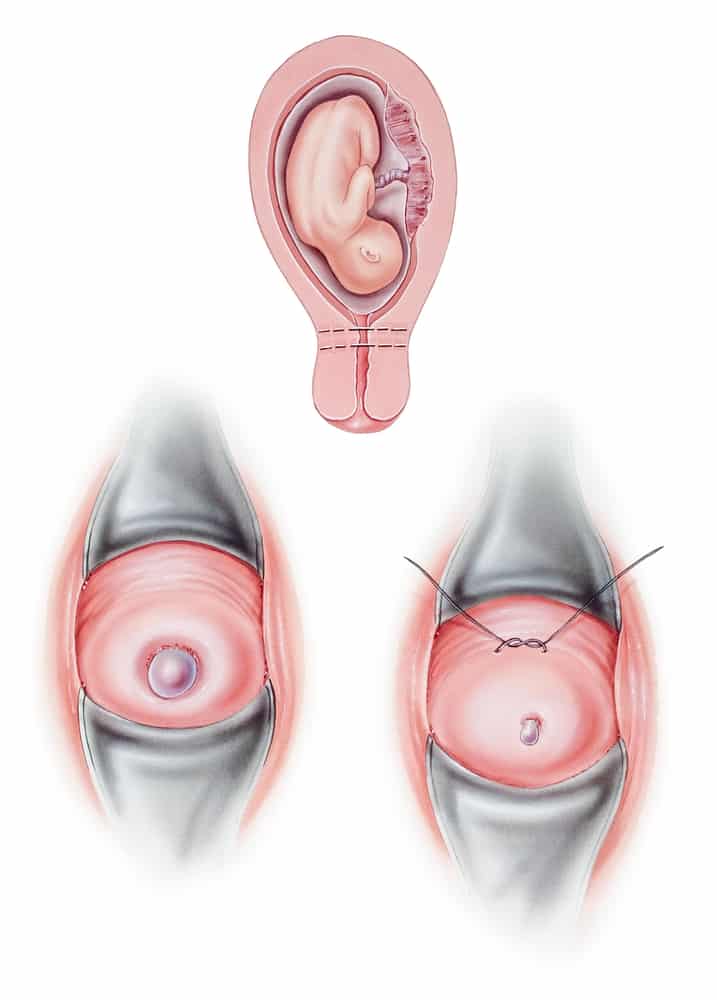
- Complete: This occurs when the placenta completely covers the cervix. When this happens, every part of the cervical opening is blocked or covered by the placenta
- Partial: In this instance, the placenta only partially covers the cervix. That is, only a part of the cervix is covered by the placenta.
- Marginal: This occurs when the placenta is located adjacent to the cervix, but not completely covering it. In fact, scans show that the placenta lies adjacent to the cervical opening
Risk Factors for Placenta Previa
Some of the factors that predispose a woman to placenta previa are:
- Maternal age greater than 35 years
- Multiple gestation
- Cigarette smoking or use of cocaine
- Number of previous deliveries
- A previous history of any of the following:
- C-section delivery
- Placenta previa
- Any surgical procedure involving the uterus
What Causes Placenta Previa?
In most cases, the factors that predispose a woman to placenta previa are either uterine or placental.
The Uterine Factors
With the uterine factors, there’s an underlying abnormality in the uterus. This causes scarring in the upper parts of the uterus, making it quite ‘uncomfortable’ for the placenta to be situated there.
These factors include:
- Previous C-section.
- Instrumentation of the uterine cavity (like D&C procedures for induced abortions or miscarriages).
- Any previous surgical process involving the uterus.
The Placental Factors
In this instance, the causal factors make the placenta increase in size to compensate for reduced function. When this happens, a larger placenta increases the risk of developing placenta previa during pregnancy.
Some of these placental factors include:
- Multiple gestation (i.e. pregnant with more than one baby at a time).
- Living at high altitudes (the oxygen available at high altitude is low, hence, the placenta does more work delivering oxygen to the fetus).
- Smoking
Diagnosing Placenta Previa
Thankfully, this condition is diagnosed easily during an ultrasound scan. Most times, this occurs during your routine antenatal clinic visit or doctor’s appointment.

In other cases, medical experts can make a diagnosis of placenta previa whenever a woman complains of any of the symptoms mentioned in this article.
During your antenatal clinic, your doctor would use an ultrasound machine to observe your little one (and the placenta). With this, he/she can see the exact location of your placenta and determine if you have placenta previa.
In women who are experiencing the symptoms of placenta previa like bleeding, it is really important to conduct an ultrasound scan before a physical examination to prevent further bleeding.
How To Treat Placenta Previa
There is no drug that cures placenta previa. However, the condition is managed with proper medical care.
In most cases, the goal of treatment or management is to limit bleeding in order to help you get closer to your due date safely. To achieve this, your doctor may prescribe drugs that prevent premature labor. With these drugs, the contractions that cause bleeding are greatly reduced.

To further reduce the symptoms, you may also get a corticosteroid prescription which helps your baby develop faster, even if he/she is not up to term. Eventually, your doctor would schedule a C-section when your baby is safe enough to join you in this world.
However, if the bleeding is heavy and incessant, an emergency C-section would be scheduled even if the baby is not up to term.
Furthermore, the treatment option for placenta previa depends on:
1. The Volume of Blood Loss.
If the bleeding is light, you’d be placed on bed rest and restricted from sex during this period and heavy exercise. However, if the bleeding is heavy, you may be given a blood transfusion to make up for the blood loss.
2. Your Expected Delivery Date
The closer you are to your due date, the better. This is because your baby will have a greater chance of survival, even if you have to undergo an emergency C-section.
3. The Position of The Placenta & The Baby
During pregnancy, positions are really important.
The position of the placenta and your baby would determine the method of treatment because your doctors would consider the best possible option for your and your little one before making any decision.
Complications of placenta previa
Sadly, placenta previa may become worse as the pregnancy progresses. In fact, it may result in life-threatening conditions for the mother and the baby.
Placenta previa complications for the mother
In some cases, placenta previa may present with other placental or umbilical cord conditions. This can eventually cause growth retardation or breech presentation of the baby.
Placenta previa bleeding also increases the risk for preterm premature rupture of membranes (PPROM), which can lead to premature labor.
In other instances, placenta previa may cause placenta accreta; a condition that occurs when the placenta grows too deeply into the uterus. When this happens, it becomes very difficult to separate the placenta from the uterus during delivery.
Sadly, placenta accreta is life-threatening and may require surgical removal of the uterus (hysterectomy) during a C-section.
Placenta previa complications for the baby
In babies, placenta previa may cause any of the following conditions that lead to premature birth:
- Low birth weight: resulting from reduce nutrient supply.
- Fetal breathing problems: due to reduced oxygen supply.
- Birth Injuries like Cerebral Palsy.
Conclusion
Finally, it is important to remember that attending regular ante-natal clinics would help your doctor identify any of the symptoms or possible causes of placenta previa.
Also, if you notice any of the symptoms mentioned in this post, please contact your doctor ASAP.
We are here for you, Mama.
References
Shobeiri, F., Jenabi, E., Karami, M., and Karimi, S. (2017). Determinants of placenta previa: a case-control study. Biomedical Research and Therapy, 4(06), 1411-1419. Accessed on 25th September, 2021 from https://doi.org/10.15419/bmrat.v4i06.182
Rao J , Fan D , Zhou Z, Luo X, Ma H , Wan Y, Shen X, Lin D , Zhang H, Liu Y and Liu Z (2021). Maternal and Neonatal Outcomes of Placenta Previa with and without Coverage of a Uterine Scar: A Retrospective Cohort Study in a Tertiary Hospital. International Journal of Women’s Health. Volume 2021:13 Pages 671—681. Accessed on 25th September, 2021 from https://doi.org/10.2147/IJWH.S310097
Jing L, Wei G, Mengfan S and Yanyan H (2018). Effect of site of placentation on pregnancy outcomes in patients with placenta previa. PLOS ONE 13(7): e0200252. Accessed on 25th September, 2021 from https://doi.org/10.1371/journal.pone.0200252