Are you pregnant? Yes? Then you may be at risk for diabetes!
How does this happen?

Gestational diabetes is a form of diabetes that appears only during pregnancy. As strange as it may sound, studies show that 6-7% of pregnant women will develop this form of diabetes during the course of their pregnancy.

What causes gestational diabetes? Are the symptoms obvious? Is it possible to keep you and your baby healthy after a diagnosis?
Read on to find out!
What Causes Gestational Diabetes?
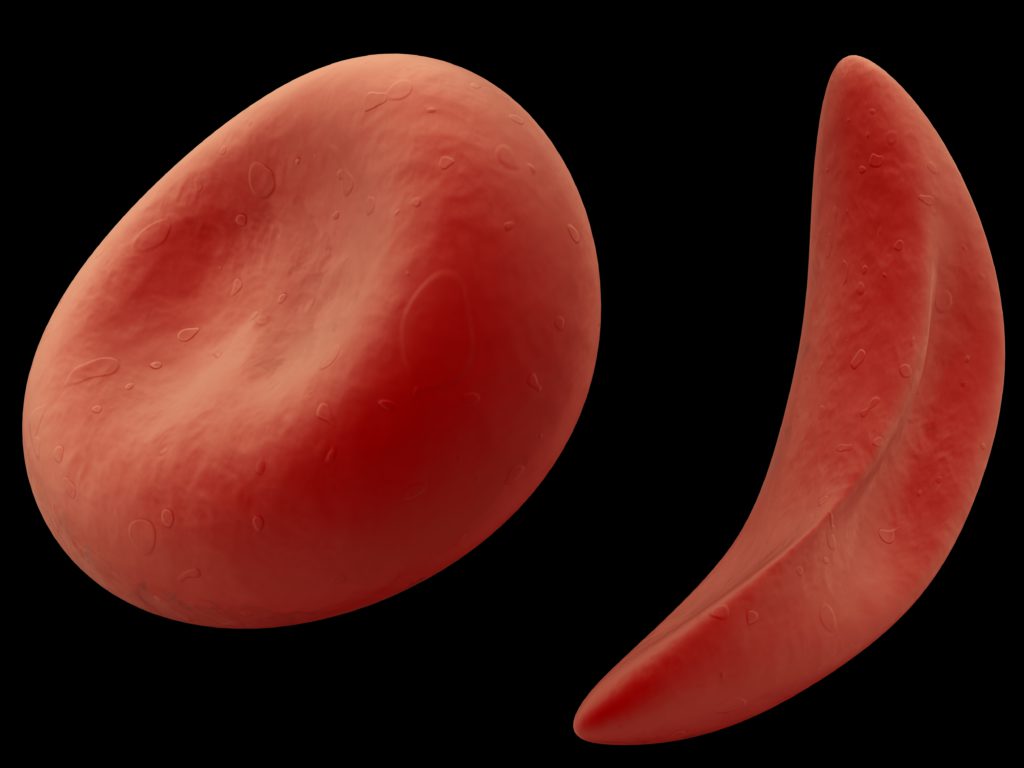
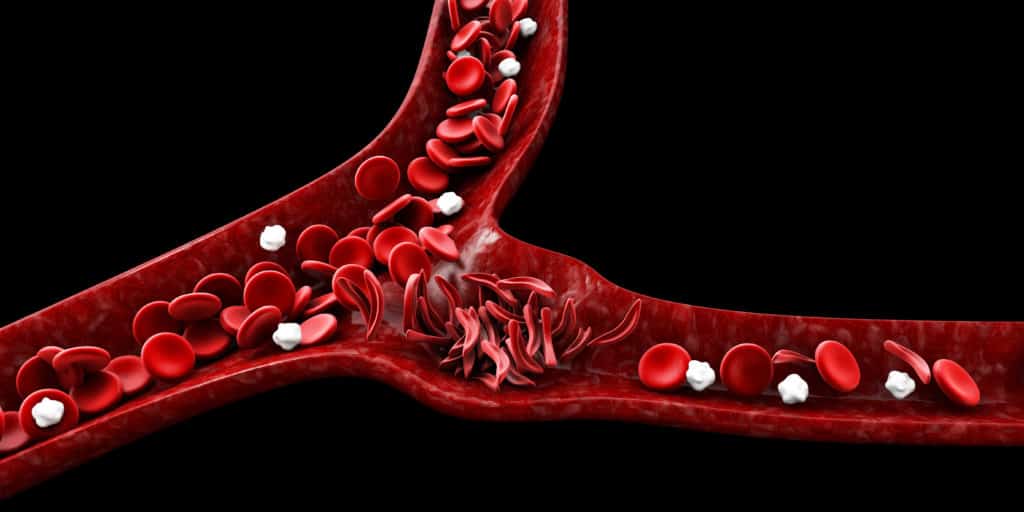
Our body releases a hormone called Insulin every time we have a meal.

This hormone helps to break down fats and carbohydrates, turning the sugar from our food into energy. At times, hormones from the placenta can prevent the production of insulin and sugar cannot be broken down properly.
Therefore, excess sugar remains in the blood and causes gestational diabetes. Gestational diabetes usually starts around the 24th to 28th week of pregnancy.
If not managed properly, this sustained rise in blood sugar can cause damage to the nerves, blood vessels and organs in your body.
Risk Factors For Gestational Diabetes
Although it is not certain why some women get gestational diabetes while others do not, there are some factors that places anyone at risk of this condition:
- Obesity
- High levels of tummy fat
- Age (Women older than 35 years)
- Polycystic ovarian syndrome
- Family history of diabetes
- Personal history of Gestational Diabetes
- History of delivering large babies (more than 9pounds/4.1kilograms)
- Sendentry Lifestyle
- Race: Sadly, being black places you at a higher risk of this condition.
Symptoms Of Gestational Diabetes
Many women who develop gestational diabetes during pregnancy may not notice any symptoms. Most women find out after they have been tested for the condition.

However, some signs you should watch out for are:
- Incessant thirst.
- Frequent urination and in large amounts
- Persistent Fatigue
- Sugar in the urine during a dipstick test
- Nausea
- Blurred vision
- Recurrent vaginal, bladder and skin infections
Your doctor will test you for gestational diabetes during your routine antenatal check ups. This is done between 24-28 weeks if you have never had it before or at your first visit if you had it in your previous pregnancy. This test is called an OGTT (oral glucose tolerance test).
How Does Gestational Diabetes Affect You and Your Baby?
If left unchecked, gestational diabetes could put you at risk for:
- Preeclampsia
- Miscarriages and pregnancy loss
- Increased risk of having a baby by caesarean section.
- Stillbirth
On the other hand, it puts your baby at risk for:
.Jaundice ( yellowing of the eyes and skin)
- Breathing difficulties
- Macrosomia; a condition where a baby is too large and the head too big for a vaginal delivery.
- Low blood sugar levels
- Low calcium levels
- Issues with the formation of organs such as the heart
- Obesity
- Type 2 diabetes later in life
However, mothers who follow their obstetrician’s advice and recommendations for either medication or dietary changes do not have to worry about these risks.

Gestational diabetes can be adequately managed with proper diet and exercise. In some cases, supplementary insulin as injections may be recommended. Other times oral tablets are given to help control your blood sugar through other mechanisms .
A diagnosis of gestational diabetes can be overwhelming. However, there is no need to despair as it can be easily controlled so that you have a safe and healthy delivery.
Your pregnancy will need to be monitored more closely eg. more frequent antenatal visits. Follow your doctors advice at all times. Maintain a healthy diet, and remain physically active. Be consistent with your medications if you have any.
As long as you follow the guidelines above, you and your baby will be fine.
References
- The Centers for Disease Control and Prevention, Prevalence Estimates of Gestational Diabetes Mellitus in the United State, 2014.
- Centers for Disease Control and Prevention, Diabetes During Pregnancy, June 2018.
- US Department of Health and Human Services, National Institute of Diabetes and Digestive and Kidney Diseases, Gestational Diabetes.
- National Institutes of Health, National Library of Medicine, Hemoglobin A1C (HbA1c) Test, November 2018.
- JAMA Internal Medicine, Lactation Duration and Progression to Diabetes in Women Across the Childbearing Years, The 30-Year CARDIA Study, March 2018.
- Shutterstock