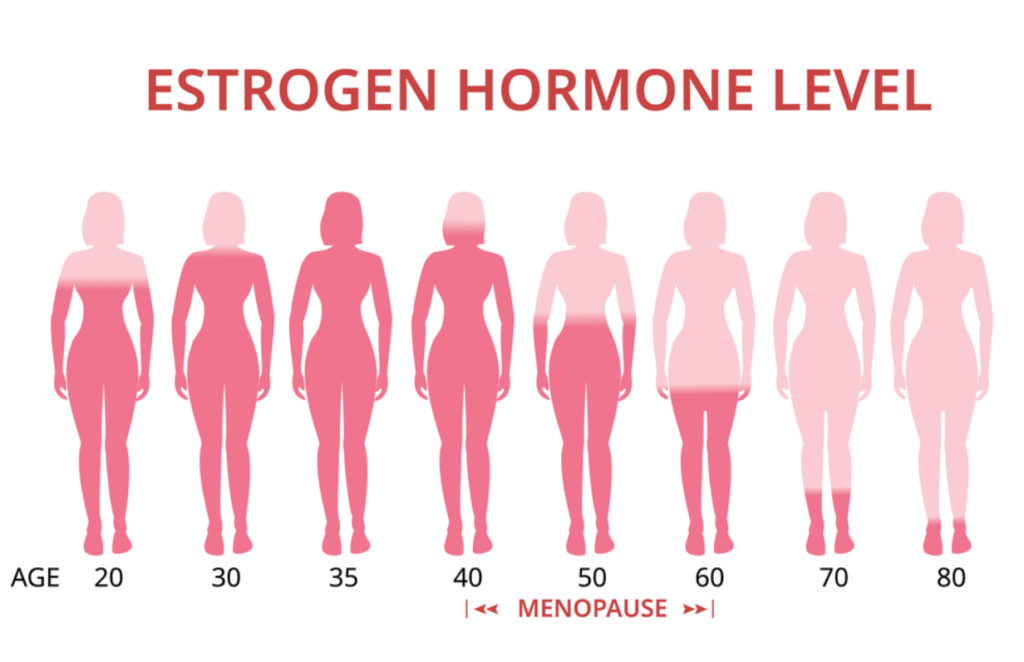
Menopause is a normal and natural stage in the life of a woman. It is the period during which menstruation stops. At this stage, there is also a slow decline in the body’s reproductive hormone levels, leading to an imbalance between these hormones. As a result, women at this stage experience the various symptoms of menopause. Thankfully, this article contains 12 of the best menopause tea options to deal with these symptoms.

Perimenopause is the period before menopause. It is accompanied by symptoms such as hot flashes, vaginal bleeding and dryness, mood changes, loss of hair, anxiety, difficulty in sleeping, weight gain, and some others. Eventually, most of these symptoms tend to subside during actual menopause.
There are natural ways to ease some of the menopause symptoms. One of such ways is making and taking the right tea. This article provides you with 12 of the best teas to relieve those stressful menopause symptoms.
Do Teas Relieve Menopause Symptoms?
The efficacy of teas in helping to relieve menopause symptoms has not been extensively studied. From the few studies available, experts agree that certain teas can relieve menopause symptoms while others are unable to.
As a result, it is very important to consult with your doctor before selecting a tea brand to treat your menopause symptoms.
12 Best menopause Teas For You
As we mentioned earlier, tea can be an effective natural remedy for various menopausal symptoms. In fact, tea is a relatively healthy and less expensive option for relieving those symptoms.
Some of the best tea options to choose from include:
1. Red clover tea
Red clover treats hot flashes and night sweats during menopause. In addition, studies show that it contains ingredients that manage postpartum hypertension, improve bone strength, and boost immunity.

Furthermore, Red Clover Tea contains isoflavones (particularly phytoestrogens), a compound that is structurally similar to estrogen, hence, its effectiveness in helping to relieve menopause symptoms. Nonetheless, experts are still waiting on the result of more scientific studies to properly identify the side effects of this seemingly important tea option.
2. Valerian Root Tea
Some studies have suggested that valerian root tea can be useful in helping to relieve menopausal symptoms such as insomnia, anxiety, stress, headaches, and hot flashes.
However, pregnant women and breastfeeding moms should completely avoid the valerian root tea during this stage of their lives. It is also important to avoid combining this tea with alcohol or using it for a very long time.
3. Black Cohosh Root Tea
This is one of the most studied herbs. Research has found that black cohost root can help relieve hot flashes, insomnia, and vaginal dryness associated due to menopause. In addition, this article contains the best lubricants to use for menopause dryness.
However, there’s a need to conduct more research to ascertain the safety and efficacy of this tea option. Based on current studies, the side effects are mild and often related to the gastrointestinal system. As it is with the valerian root tea, pregnant women, hypertensive patients, and people with liver problems should completely avoid this tea option.
4. Ginseng tea
Ginseng also reduces various menopause symptoms. This tea can help reduce the occurrence and the severity of hot flashes and night sweats. Furthermore, it also increases sexual arousal and may improve the quality of sex in menopausal women.
Some of the side effects of ginseng tea include headaches, nervousness, and jitteriness.
5. Sage tea
Recent research shows that sage extract improves concentration, and reduces hot flashes, night sweats, fatigue, and panic in menopausal women, although the focus was on a really small population.

6. Dong Quai Tea
Dong Quai tea helps balance and regulate estrogen levels in the body of women starting menopause. Furthermore, this tea option reduces cramps associated with premenstrual syndrome (PMS) and also ease pelvic pain in menopausal women.
Furthermore, this tea is not suitable for women preparing for surgery.
7. Licorice Tea
Licorice tea also reduces the frequency and severity of hot flashes in menopausal women because it contains many active ingredients like isoflavonoids, steroids, and terpenes.
It also has some estrogen-like effects and may be effective in improving respiratory health and reducing overall stress. However, studies also shows that licorice tea may have some adverse effects when combined with other drugs. Therefore, it is important to consult with your doctor to get the right menopause tea option.
8. Ginkgo Biloba Tea
This tea contains phytoestrogens and increases estrogen levels and solves hormonal imbalances in menopausal women. It is also useful in cases of low libido in menopausal women. Furthermore, it can also improve PMS symptoms and ease mood swings.
On the other hand, Ginkgo biloba may interfere with blood clotting in certain people. Some other side effects include headaches, gastrointestinal problems and allergic reactions.
9. Chasteberry Tree Tea
Drinking chasteberry tree tea can reduce breast pain during menopause and hot flashes in menopausal women. It contains progesterone which helps to maintain a healthy balance between fluctuating levels of estrogen and progesterone in this period.

Women who are using hormones for birth control or hormone replacement should not take chasteberry. Also, patients with hormone-sensitive diseases such as breast cancer should avoid it. In addition, women on antipsychotic medications or medications for Parkinson’s disease should also not drink chasteberry tea.
10. St. John’s Wort Tea
St. John’s wort tea may be useful to treat menopause symptoms, however, there’s still a need for further research on its effectiveness. In addition, this tea may be useful in treating inflammation and certain nervous disorders.
11. Red raspberry Leaf Tea
This tea lessens the heavy menstrual flow that accompanies the onset of perimenopause. It is considered safe to drink during the transition from perimenopause to menopause.

12. Fennel tea
Fennel is a member of the carrot family and also has some anti-inflammatory properties. This tea can help menopausal women in managing problems with sleep, sex, depression, and anxiety.
A Final Note From Edie & Amy
Menopause is a natural and normal stage in every woman’s life, although it may come with some symptoms that may negatively affect an individual’s health. Most of the scientific research done on menopausal teas is inconsistent and incomplete. Therefore, you’ve got to be really careful with every decision regarding menopause tea.
Also, due to the way these menopause tea options interact with the body and with other drugs, you should not use them unless you have discussed them with your doctors. This helps to reduce side effects and prevent damage to the health.
References
Kheirkhah, M., Naieri, S. D., & Tabari, N. S. (2018). The effect of herbal tea capsule on menopause hot flashes. Journal of family medicine and primary care, 7(5), 1074–1078. https://doi.org/10.4103/jfmpc.jfmpc_332_17