Some women don’t get to know they are pregnant until a few weeks or even months after conception. It is possible that this bundle of joy will start developing inside you and you won’t know except you’re very familiar with the early signs of pregnancy. Since the time frame between conception and getting to know you’re pregnant is a little wide, an accurate estimation of the conception date becomes difficult.
The conception date is the date your baby was conceived. It can be a little difficult, if not impossible for you to know this date by yourself. This is because you can’t tell when the sperm actually fertilized your egg. In fact, you can have sperms living in your womb for about three to five days following intercourse.

As you continue reading this article you will get to know why it is important to know your conception date, how you can know it, and the accuracy of ultrasound in knowing your conception date.
Table of contents
How early can you know you are pregnant?
You can go for a pregnancy test if you think you have missed your period or you have symptoms related to early pregnancy. The earliest time to take a pregnancy test is two weeks after fertilization has taken place. This is because, at that time, your body is already responding to the hormonal changes associated with pregnancy.
Thankfully, you can conduct a pregnancy test at home using a pregnancy test strip.

Why Is Your Conception Date Important?
There are a couple of reasons why you should know your conception date. Knowing your conception date is important because it helps to calculate your due date. With an accurate conception date, your health care provider can use a mathematical formula to calculate when it’s likely for you to deliver. If you don’t get to know your conception date, only an approximate delivery date will be used based on your last menstrual period (LMP).
You can also read this article to learn how to calculate your conception and baby due dates.
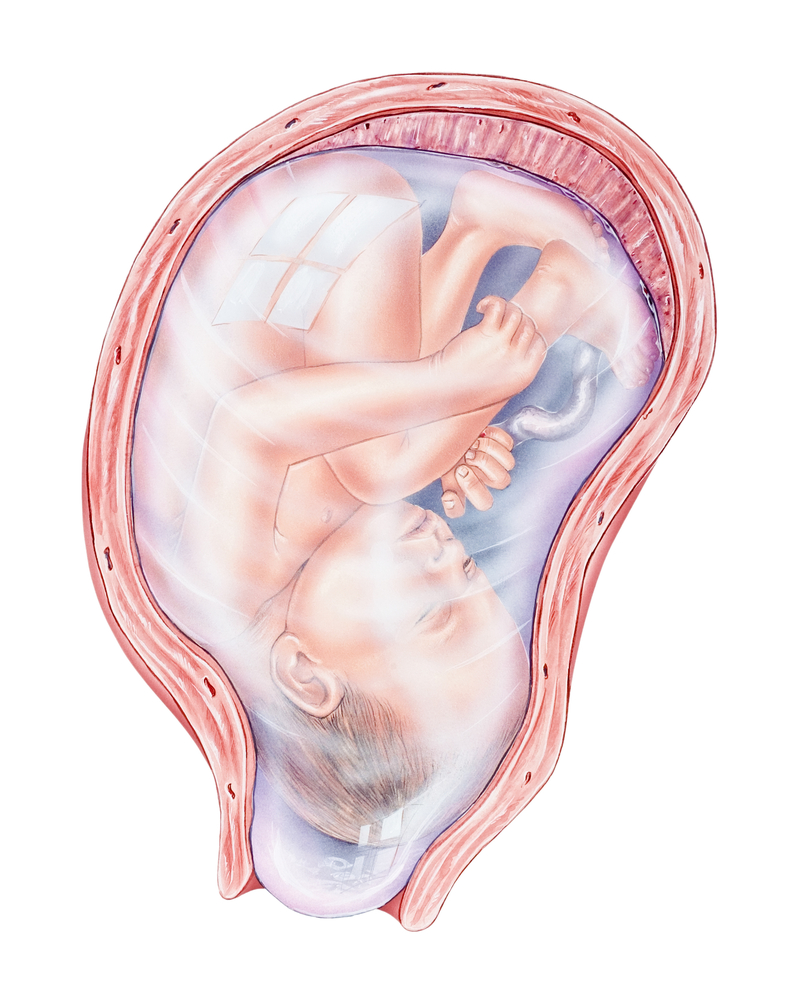
Another important reason why you should know your conception date is that it helps to keep track of your baby’s development. Your baby’s body development in the womb depends on the number of weeks he or she has spent there. Different parts of the body develop at different times. Therefore, knowing your timeline would help you follow the stages of pregnancy and prenatal development.
How can you know your conception date?
There are different methods to know or calculate your conception date. One of them is using your LMP. If you remember your LMP, it is easy to use mathematical formulas to know the range of days conception took place.
Read this post to see the mathematical formula to calculate conception dates.
This method has a number of shortfalls. Firstly, it is not possible to find the actual conception date, as one only gets a range. Secondly, some women don’t remember their LMP. This makes it difficult for the health care provider to estimate their conception date.
Another method to find conception dates is via an ultrasound. It is a medical device that uses sound waves to look inside your body and convert these waves to images.
During an ultrasound, a transducer at the top of your stomach emits sound waves that bounce off on your baby in the womb. The transducer then picks the echoes produced and translates them into the image of your baby and this is what you get to see on the screen.

In addition to being really easy to conduct, ultrasounds are safe for both the mother and the child.
How do ultrasounds determine conception dates?
Ultrasounds can tell how far you’ve gone in pregnancy. This happens by comparing your baby’s growth with standard growth patterns for babies. While in the womb, babies grow really fast and the growth pattern is similar for babies all around the world.
When an ultrasound converts the sound waves to images on the screen, the image that pops up is compared with the available standard growth patterns for babies. The appearance of some organs or parts of the body also tells the possible week your pregnancy might be.
The baby’s size can also be measured alongside certain other distinguishing features since specific parts or organs of the body grow at different rates and at different times. With a careful analysis of all these factors, an accurate estimate of the conception date is gotten.
Are ultrasounds really accurate in knowing your conception date?
Ultrasounds are very accurate in determining the date you actually conceived your baby. It measures the crown to rump length of your baby (i.e. head to buttocks) and this length can be used to estimate how old your baby is in the womb.
This can be traced back or compared with standard patterns to tell your conception date.
How can you get an ultrasound?
Most health care facilities, especially obstetrics and gynecology clinics have ultrasound machines. Some even offer free ultrasound scanning during antenatal clinics. With effective ultrasounds, you can easily track the progress of your pregnancy.
Conclusion
If you think you are pregnant or you recently discovered that you are pregnant, it is good that you get to see a doctor. It is very important to know your conception date as you monitor the progress of your pregnancy. The accuracy of the available methods of estimating the conception date differs.
Nevertheless, with an ultrasound, you’re as sure as you can ever be.