Planning is really important, especially when it relates to childbirth. It requires great and adequate preparation on the part of the parent. Thankfully, family planning provides a great means to plan and prepare for the coming of a new child and also to prevent unplanned pregnancy.
Family planning methods are of great health importance in every society. However, it is super important to have a solid understanding of the benefits and possible disadvantages of any family planning method.
This article will help you understand what family planning is; the types of family planning methods available, and the advantages or disadvantages of family planning.

Table of contents
What does family planning mean?
The primary goal of family planning is to prevent unplanned pregnancies. Family planning entails the different methods by which pregnancy is prevented. It can be through sexual practices, use of barriers, drugs, devices, or even surgical procedures. In short, we can say that any act, practice, or device that prevents a woman from getting pregnant is a contraceptive.
Family planning does not just prevent a woman from getting pregnant, it also considers the health status of the woman and her readiness to start a family. Furthermore, family planning can be used to space pregnancies. that is you can space pregnancies A and B with effective family planning methods.
Types of family planning methods
There are different types of family planning methods. Thankfully, these methods can be placed into two broad groups:
- Natural or traditional methods: This includes knowing your calendar and having sex during your safe period. It also includes the withdrawal method. In the withdrawal method, the man pulls out his penis from the woman’s vagina before ejaculating. However, the withdrawal method is largely ineffective and isn’t one of the top contraceptive options for males.
- Artificial or modern methods: There are several modern methods of contraceptives. They include the barrier methods (use of male and female condoms, cervical cap, and diaphragm); contraceptive pills, implants, and surgical methods.
Advantages of family planning
Reduces unsafe abortions from unintended or unplanned pregnancy.
Pregnancy is a great delight when you and your partner are ready for it.
A larger percentage of women who become pregnant without planning for it end up aborting the pregnancy. This is because either or both parties involved may not be ready for it at the moment or may not have the capacity to shoulder the responsibility of a new child.
Thankfully, family planning helps to reduce this by ensuring that the woman tries to be pregnant when the family is ready for a new addition.
Reduces maternal morbidity and mortality.
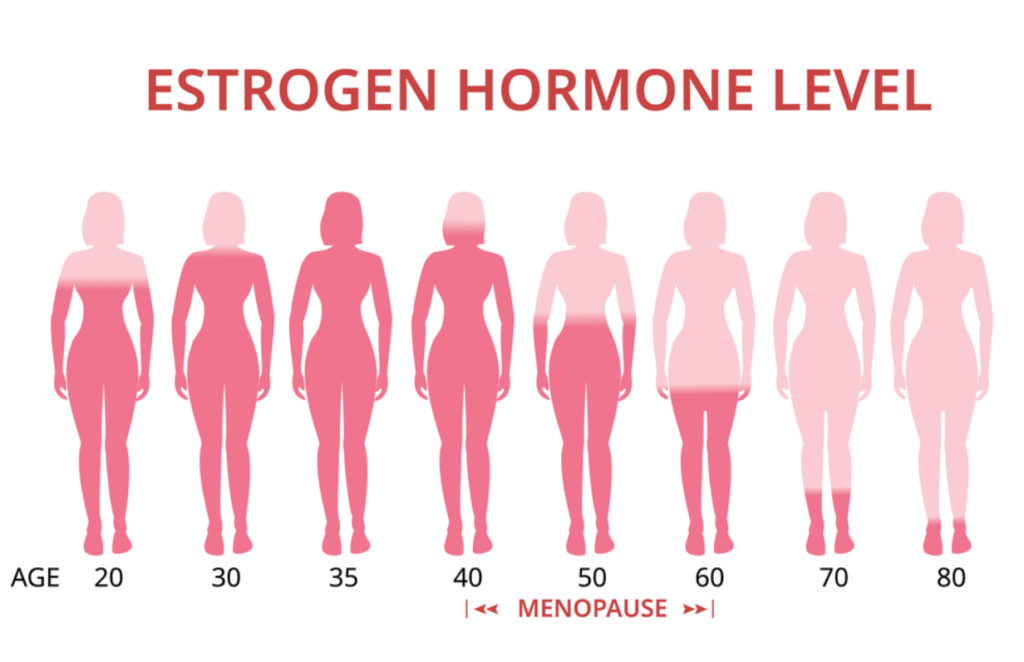
Family planning prevents unintended pregnancies, thereby reducing maternal mortality and morbidity. It allows spacing of pregnancies and delaying of pregnancies in young girls who are at an increased risk of health problems that may arise from early childbearing. Furthermore, it protects older women from pregnancy-related health risks.
It helps to limit the size of the family.
Family planning helps couples who wish to limit the number of their family do so. It also helps them space the birthing period for as long as they want.

Reduces newborn and infant mortality.
Some of the world’s highest infant mortality rates are caused by closely spaced and ill-timed pregnancies and birth. With effective family planning, this issue can be controlled.
Reduces adolescent pregnancies.
Adolescents who become pregnant are at risk of preterm and low birth weight babies. They also have a higher rate of neonatal mortality. These and other adolescent pregnancy-related issues can be reduced with proper family planning. Also, preventing unintended pregnancy in adolescents helps to improve their sexual and reproductive health and also their social and economic wellbeing.
Disadvantages of family planning
Cost
The cost of family planning depends on which method you are going for. The cost of maintaining some family planning methods is high. The methods that are not permanent need to be replaced daily or monthly, e.g. contraceptive pills. The cost of getting the very effective ones like intrauterine devices (IUD) is very expensive. In fact, if you don’t have insurance, you may not be able to get one.
To solve this problem, certain contraceptive and family planning options have now become completely free in government hospitals in some countries like Nigeria.
Irreversibility
The surgical family planning methods (hysterectomy, tubal ligation, and vasectomy) are irreversible. This means that if you change your mind in the future about having babies, you may not be able to be pregnant again. There are no means of reversing the effect once you opt for them.

Side Effects
Many women who opt for contraceptive pills are at risk of many side effects including breast tenderness, depression, headache or migraine, irregular bleeding, nausea, change in appetite, weight gain, hair loss, or increased hair on the face or body, change in sexual desire and vaginal irritation.
Some of the pills can also put women at risk of certain cancers. A common side effect of most family planning procedures is pain. The convenience of consistently using birth control pills is also a problem.
Risk of failure
Some of the family planning methods are not a hundred percent effective. Certain studies show that a woman may still get pregnant after using a contraceptive or family planning method. In fact, women who use contraceptive pills can still become pregnant if they skip the pills for one day.
No protection against HIV and STDs.
Most family planning methods do not provide protection against sexually transmitted diseases (STDs). As a result, people still require protection from sexually-related diseases in addition to protection from unwanted pregnancies.
Conclusion
The use of contraception is very important and useful in every society. Of course, your choice of a family planning option would go a long way in maintaining your sexual and reproductive health. Thankfully, your doctors and healthcare providers are always available to guide you to the right option for you and your partner.