During pregnancy, your body does something incredible- It grows a new, but temporary, organ called the placenta. As you expect your little one, the placenta performs various functions that aid your baby’s development during pregnancy.
At the end of pregnancy, in normal situations, the placenta would also be delivered (right after your baby is born). However, in some instances, the placenta does not deliver when it should. When this happens, there’s a lot of bleeding that may become life-threatening if the placenta is retained for more than 30 minutes.
In this article, you’d find reliable info on retained placenta; the types, causes, risk factors, symptoms, and treatment options.
Read on to learn more!
Table of contents:
- What Is A Retained Placenta?
- What Happens To The Placenta After Childbirth?
- Types of Retained Placenta
- What Causes Retained Placenta?
- Risk factors for retained placenta
- Normal Placenta Delivery
- How To Diagnose A Retained Placenta
- Retained Placenta Symptoms
- Treatment of Retained Placenta
- How To Prevent Retained Placenta
- Conclusion
What Is A Retained Placenta?
Retained placenta occurs when the placenta remains in the uterus after giving birth, especially during vaginal delivery. The entire placenta, a part of it, or its membranes can remain in the uterus. As we mentioned earlier, a retained placenta may lead to serious blood loss.

What Happens To The Placenta After Childbirth?
In childbirth, the placenta is also delivered through the birth canal after the baby has been delivered. In fact, doctors often refer to this process as the third stage of labor.
Normally, labor occurs in three stages which are:
- Contraction stage:This is the stage when your uterus begins to contract. This causes changes in the cervix that prepares it for delivery.
- Delivery stage: At this point, your baby is born.
- Placenta delivery stage: This stage occurs after the child delivery. After this, placenta delivery occurs.
Usually, the placenta is extruded within 30 minutes after the baby has been delivered. So, if the placenta remains in the uterus for more than 30 minutes after the baby has been delivered is known as a retained placenta.
Types of Retained Placenta
Basically, there are three types of retained placenta:
- Placenta adherens. This is the most common type of retained placenta. It occurs when the placenta remains loosely attached to the walls of the uterus, but the uterus does not contract enough to expel it.
- Trapped placenta. This occurs when the placenta detaches from the uterus but it doesn’t leave the body. It may result from premature closure of the cervix, which occurs when the cervix begins to close before the placenta is delivered.
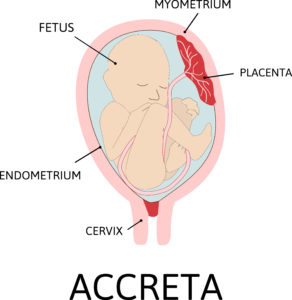
- Placenta accreta. This is a type of retained placenta that occurs when the placenta attaches to the muscular wall of the uterus instead of the lining of the uterus. This complicates the placenta delivery process, and results in severe bleeding.
What Causes Retained Placenta?
Some of the causes of a retained placenta are:
- Inadequate uterine contractions after delivery.
- An umbilical cord tear during delivery.
- The placenta attaching abnormally to the wall of the uterus (the muscular wall)
Risk factors for retained placenta
The probability of having retained placenta increases in the following instances:
- Increased maternal age (above 30 years)
- Prolonged first and second stage of labor
- A premature delivery or delivery before the 34th week of pregnancy
- Having a still birth
Normal Placenta Delivery
There are usually two options for placenta delivery following vaginal birth:
- The first is active management. This involves injecting you with oxytocin to make your womb contract. This helps to expel the placenta. This procedure may facilitate placenta delivery within 30 minutes of childbirth.
- The second is physiological management. This involves delivering the placenta without any medication or hormones. This can take up to an hour.

Your midwife or doctor may also do any of these to help you deliver the placenta:
- Help you empty your bladder
- Ask you to breastfeed your baby
- Help you massage the top of your uterus
- Ask you to change position to either sitting or squatting
If you’re having a C-section, the surgeon would take out the placenta as a part of the procedure.
Read Also:
How To Diagnose A Retained Placenta
Thankfully, the placenta has distinct features that make it easy to identify its complete removal after delivery. This way your doctor or surgeon can easily identify any case of incomplete or partial placenta delivery.
Doctors diagnose retained placenta if the placenta is not expelled within:
- 30 minutes after your baby’s delivery with active management
- 1 hour after your baby’s delivery with physiological management
Retained Placenta Symptoms
Obviously, the main symptom of a retained placenta is the failure of placenta delivery after childbirth. In other instances, pieces of the placenta may remain stuck in the uterus after childbirth, leading to infection and heavy postpartum bleeding.
If you notice any of these symptoms days or weeks after giving birth, contact your doctor:
- Fever
- Heavy bleeding
- Discharge from the vagina that contains tissue and has a foul smell
- Persistent pain

Treatment of Retained Placenta
Treating a retained placenta involves removing the entire placenta or any missing part of the placenta. In most cases, this is achieved by:
1. Manual Removal
Your doctor or midwife can remove the placenta by putting one hand into the uterus to gently pull the placenta out while placing the other hand on your stomach to help steady your uterus. It is important to note that this procedure is often done right after childbirth. To ease the pain, your doctor would prescribe anesthetics.
2. Drug Therapy
In this instance, your doctor would administer certain medications that improve uterine contractions. With these drugs, like oxytocin, your uterus would contract well enough to expel the placenta.
3. Breastfeeding
Interesting, right?
Yes, this is another one of the many benefits of breastfeeding.

After delivery, breastfeeding increases the production of oxytocin, which promotes the uterine contractions necessary to expel the placenta after childbirth.
4. Surgery
After trying all the methods mentioned above, and the placenta is still not extruded, you may need to undergo emergency surgery to remove any remnant placenta tissue.
However, this is only considered as a last resort.
How To Prevent Retained Placenta
Thankfully, retained placenta can be prevented by following routines that facilitate the third stage of labor. These include:
- Controlled Cord Traction – After delivey of your baby, the umbilical cord is cut and clamped. Your doctor or midwife then applies gentle pressure to help separate the placenta from the wall of the uterus
- Administration of synthetic Oxytocin – During labor, this medication is given immediately after delivery of your baby to help the uterus contract as you get into the third stage.
- During pregnancy, there are some things you can do to strengthen the uterine muscles and enable them contract properly when labor starts:
These actions promote proper uterine contractions during labor and facilitate the normal delivery of the placenta.
Conclusion
In conclusion, it is important to attend your antenatal clinics regularly as you expect your little one. This would provide your doctor with all the info needed to identify and manage any placenta complications during pregnancy. Furthermore, it is important to avoid the risk factors and keep an eye out for any of the symptoms mentioned in this article. You can read more on Eating Placenta here
We are always here to help you.
References
Alessandro Favilli, Valentina Tosto, Margherita Ceccobelli, Fabio Parazzini, Massimo Franchi, Vittorio Bini and Sandro Gerli (2021). Risk factors for non-adherent retained placenta after vaginal delivery: a systematic review. BMC Pregnancy Childbirth 21, 268. Accessed on 29th September, 2021 from https://doi.org/10.1186/s12884-021-03721-9
Nicola C Perlman and Daniela A Carusi (2019). Retained placenta after vaginal delivery: risk factors and management. International Journal of Women’s Health 11: 527–534. Accessed on 29th September, 2021 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6789409/#__ffn_sectitle
Heleen J van Beekhuizen, Andrea B Pembe, Heiner Fauteck & Fred K Lotgering (2009). Treatment of retained placenta with misoprostol: a randomised controlled trial in a low-resource setting (Tanzania). BMC Pregnancy Childbirth 9, 46. Accessed on 29th September, 2021 from https://doi.org/10.1186/1471-2393-9-48